Chapter 9: Low-Efficacy Stimulants
2nd edition as of August 2022
Chapter Overview
Continuing our discussion of CNS stimulants, we will turn our attention to nicotine and caffeine. These drugs are called low-efficacy stimulants because they have moderate stimulating effects compared to cocaine and amphetamines. If you pay close attention to the mechanisms of action for these drugs, you should be able to recognize why nicotine and caffeine have a less intense stimulatory effect. Keep this in mind as you read through this chapter.
Chapter Outline
- 9.1.1. Drug History and Overview
- 9.1.2. Administration and Pharmacokinetics
- 9.1.3. Mechanisms of Action and Effects
- 9.1.4. Long-Term Effects and Treatment
- 9.2.1. Drug History and Overview
- 9.2.2. Administration and Pharmacokinetics
- 9.2.3. Mechanisms of Action and Effects
Chapter Learning Outcomes
- Describe the history, administration, mechanisms of action, and effects of nicotine.
- Describe tobacco use disorder and outline treatment approaches.
- Describe the history, administration, mechanisms of action, and effects of caffeine.
9.1. Nicotine
Section Learning Objectives
- Explain the history and uses of nicotine and tobacco.
- Describe the pharmacokinetic properties of nicotine and compare smoking to vaping.
- Describe the pharmacodynamic properties of nicotine
- Explain the effects of long-term use and describe treatments for nicotine addiction.
Most people know someone who is either a current smoker or a former smoker. It may be a friend, sibling, parent, child, or even you. Because of its prevalence, smoking is the most common addiction in the U.S. and is the leading cause of preventable death—7 million people die every year worldwide from smoking, with 480,000 deaths per year in the U.S. alone (Centers for Disease Control and Prevention [CDC], 2020). In this section, we will examine nicotine, the key ingredient in cigarettes that is responsible for the pervasiveness of smoking, and why the habit can be so hard to quit.
9.1.1. Drug History and Overview
Nicotine is the major psychoactive component of tobacco. For the most part, the history of nicotine is the history of tobacco. Nicotiana tabacum is the most common tobacco plant, although nicotine can be found in other tobacco species. Tobacco plants are native to the Americas and were used by Native Americans, who valued them for their psychoactive properties. They also used the leaves to barter and trade for goods.
Tobacco use spread to Europe in the 1500s and was studied by physicians of the time. Its popular use steadily increased and by the 1600s, English settlers in Jamestown were growing tobacco as a reliable source of income. Tobacco was not only imported back across the Atlantic for recreational use, but it also served as an insecticide.
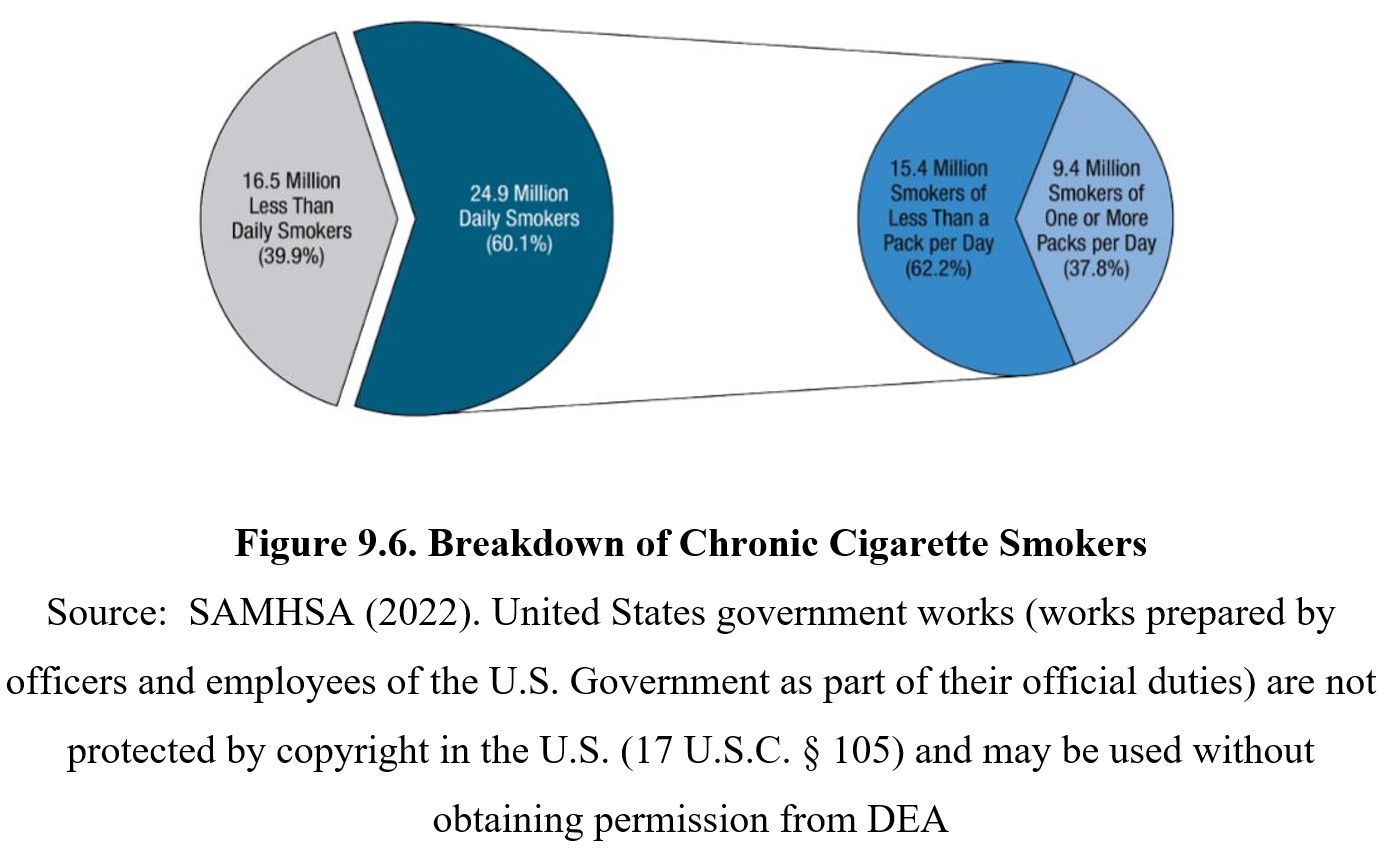
In the late 1800s, machines were invented that could roll cigarettes, fueling the modern smoking epidemic. Cigarette use rapidly rose in the early 1900s. But as smoking increased, so did evidence that link it to lung cancer and addiction. The majority of current smokers fulfill the criteria in the DSM-V for drug dependence. They have difficulty stopping smoking. They become tolerant of the effects of tobacco and need to smoke more to get the same results. They continue smoking despite being aware of its health hazards. And they exhibit craving and withdrawal signs when they stop smoking. In 1965, the U.S. government began to require warning labels on packs of cigarettes. Subsequent legislation placed restrictions on its use or imposed heavy taxes.
In recent decades, smoking rates have fallen regularly in the U.S. and other developed countries, although smoking continues to increase in less developed countries as tobacco companies focus marketing on places with fewer regulations (Dani & Balfour, 2011). According to the World Health Organization (2008), by the year 2030, over 80% of the world’s deaths from tobacco use will be in developing countries.
9.1.2. Administration and Pharmacokinetics
Tobacco is usually consumed by inhaling or chewing. There are various ways to smoke tobacco, such as through cigarettes, cigars, pipes, and hookahs. Each method varies in the amount of tobacco it contains and how the tobacco is prepared. A recent development is e-cigarettes, which allow users to inhale vaporized nicotine directly, a process known as vaping. Vaping is touted as a safer alternative to smoking, and while there are fewer recognized health risks, the discussion is more complicated because of the newness of e-cigarettes and insufficient research. Watch this video to learn more about vaping and how it differs from traditional smoking:
Smoking vs Vaping [4:19]
Nicotine is a lipid-soluble drug, meaning it is readily absorbed by the body. Nicotine that is smoked or vaped is absorbed by the lungs, while in the case of chewing tobacco and snuff, it is absorbed through the mucous membranes in the mouth or nose. As you can see in the graphs below comparing the nicotine concentration of different methods, absorption is faster through the lungs.
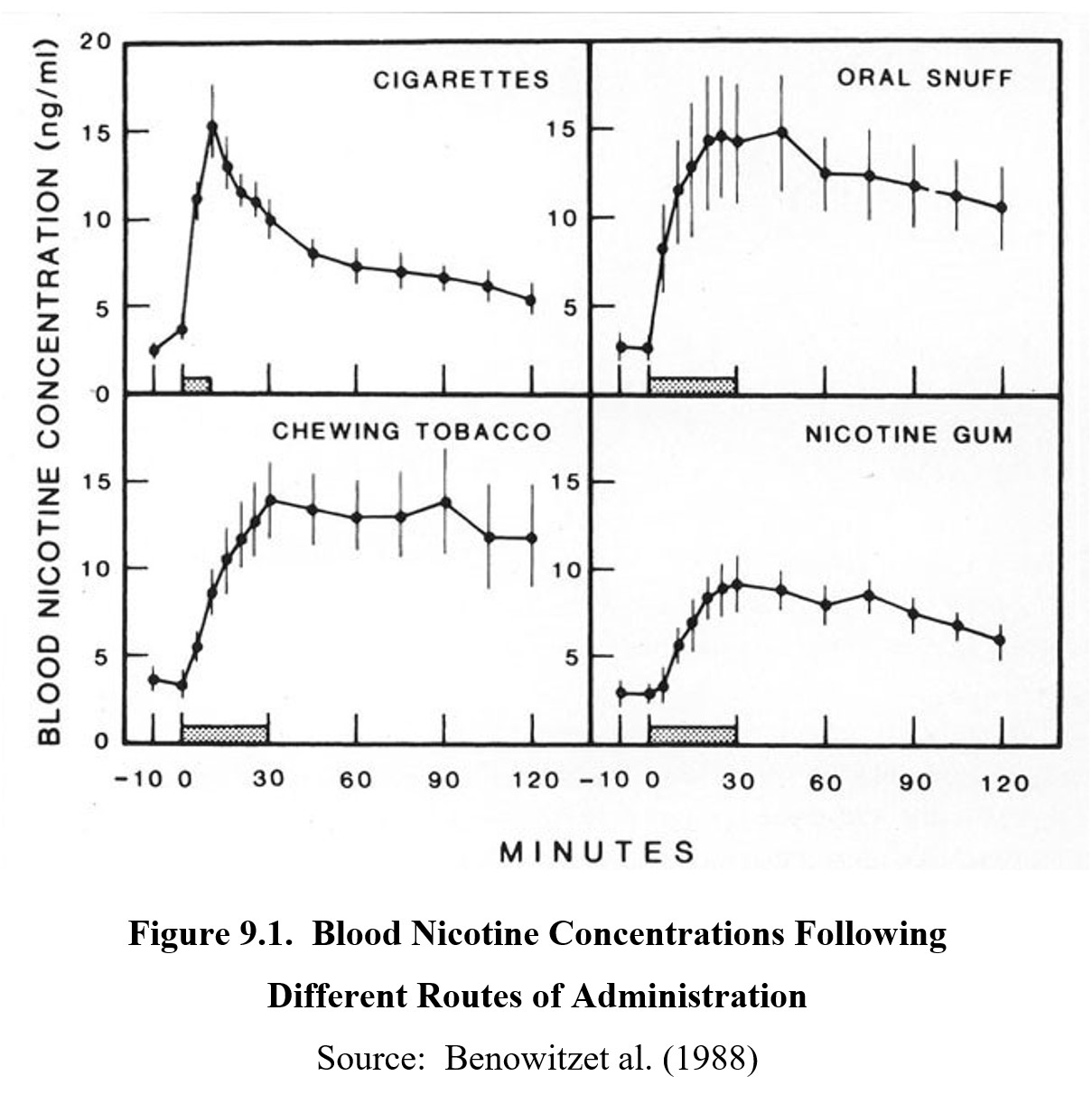
Aside from the lungs or mucous membranes, nicotine can also be absorbed transdermally, as in the case of nicotine patches used for smoking cessation. Blood concentrations usually reach 12-16 ng/ml from tobacco products. However, smoking allows users to titrate, or adjust the dose of nicotine by inhaling more frequently or deeply. Once in the bloodstream, nicotine is capable of crossing the blood-brain barrier.
Most of the absorbed nicotine is metabolized into cotinine, a partial agonist metabolite, by the enzyme CYP2A6 in the liver. The half-life of nicotine is 1-2 hours, while cotinine has a half-life of about 16 hours. Because of cotinine’s longer half-life, its presence in urine or blood is used as an indicator of recent nicotine use.
Inhalation of cigarette smoke becomes a route of administration of nicotine in others beside the active smoker. Firsthand smoke is how nicotine enters the body of the smoker. Secondhand smoke is inhaled by other people including non-smokers. Thirdhand smoke is smoke residue that settles on clothing, bedding, furniture, and other surfaces.
9.1.3. Mechanisms of Action and Effects
Recall that the neurotransmitter acetylcholine (Otto Loewi’s vagusstoff) acts on two types of cholinergic receptors: muscarinic receptors; and nicotinic receptors. The latter is named after nicotine, which produces most of its effects by being a full agonist on nicotinic receptors. Nicotinic receptors are ligand-gated ion channels that allow sodium, calcium, and potassium ions to pass through when opened. The result is an excitation of postsynaptic receptors.
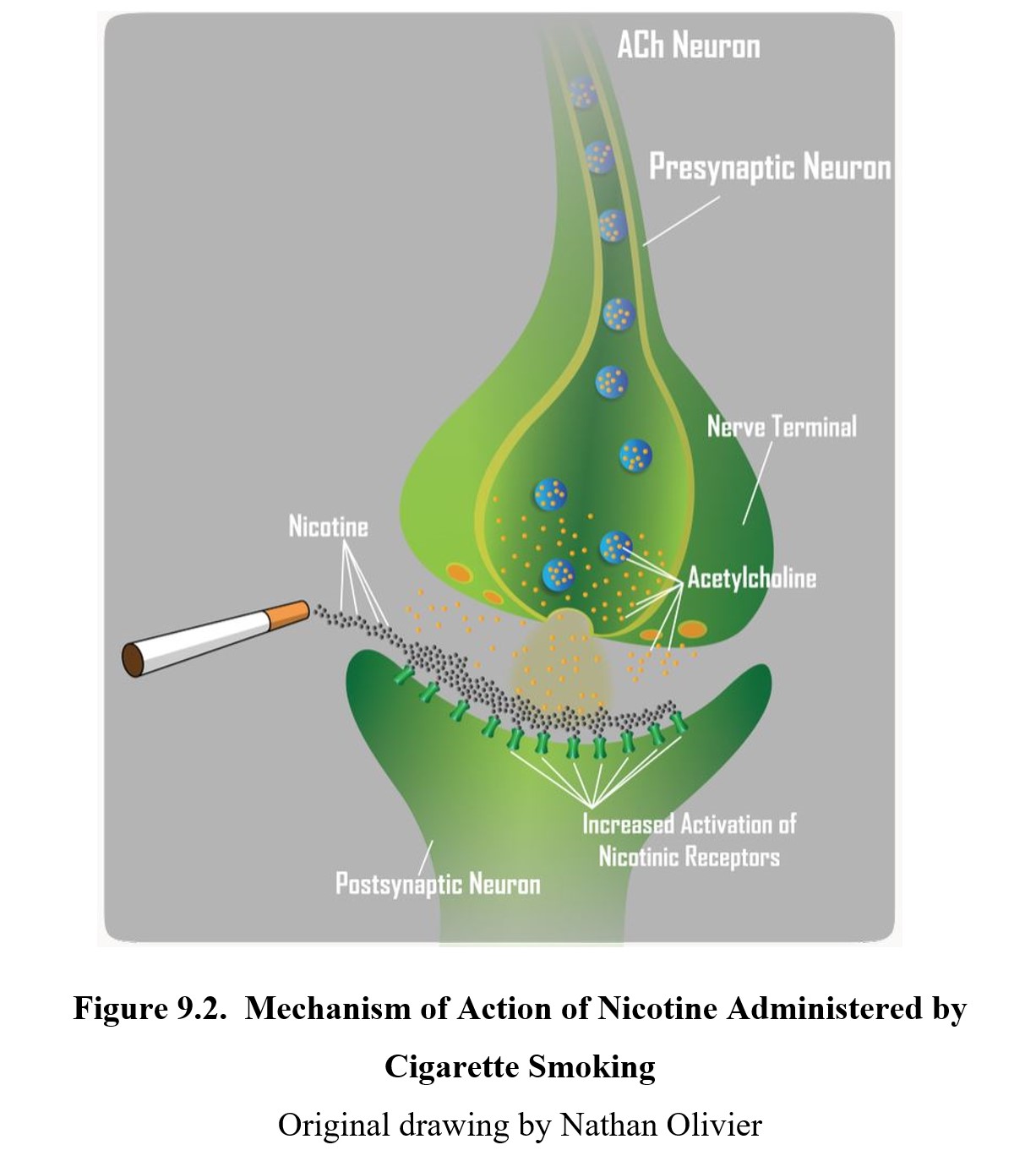
Nicotinic receptors are found on sodium and calcium ion channels and are present both centrally and peripherally. Nicotinic receptors modulate neurotransmission in a broad range of neuronal pathways. The effects of nicotine are excitatory on these systems leading to a variety of drug effects. Below is a list of the significant transmitters that are released by nicotine and their subsequent effects:
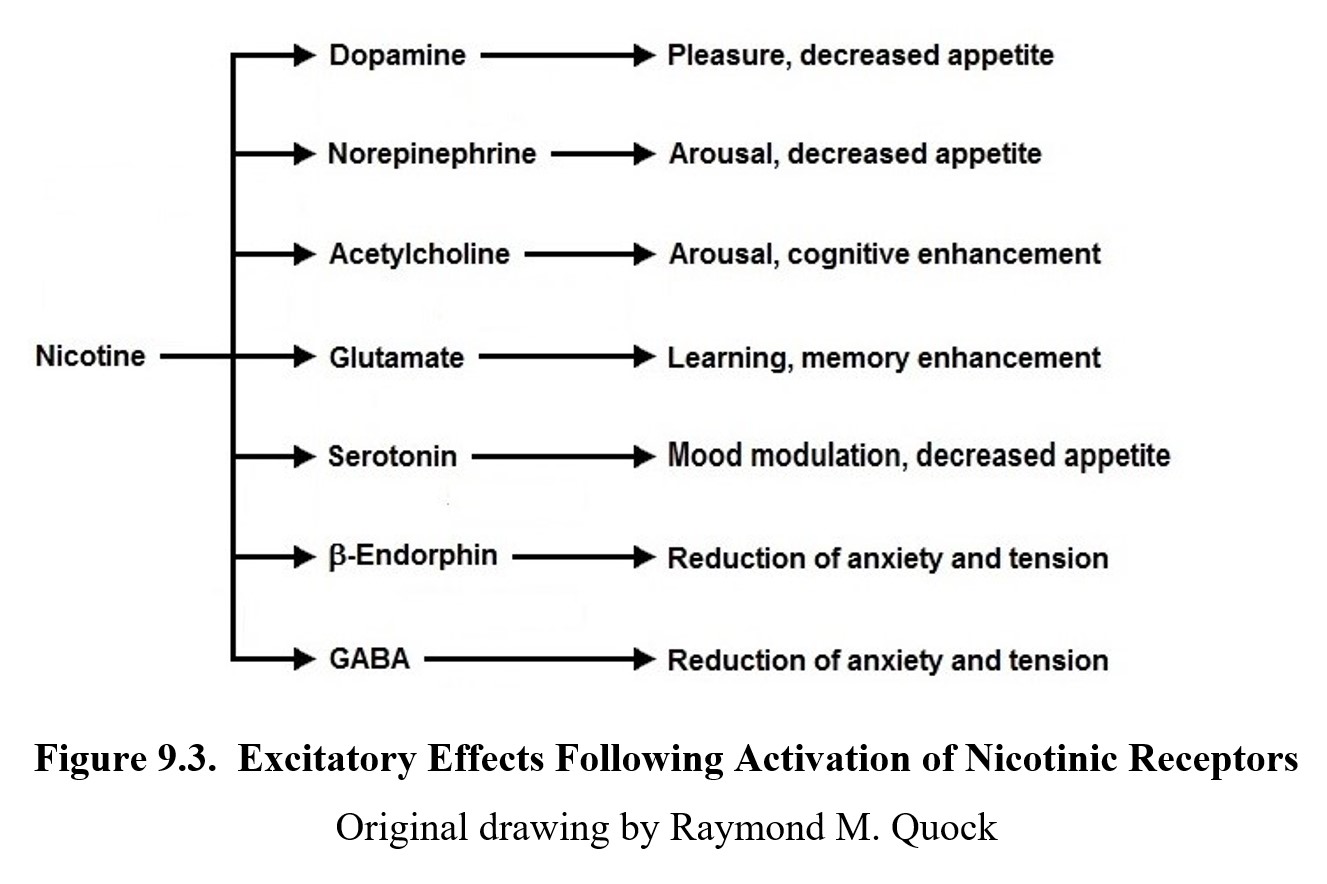
In the brain, activation of excitatory presynaptic nicotinic receptors results in a wide range of central effects ranging from relief of anxiety, regulation of mood, and changes in appetite, alertness, and cognition. Nicotinic receptors also increase dopamine release in the mesolimbic pathway, particularly in the ventral tegmental area and nucleus accumbens, which accounts for its addictive properties. Tobacco smoke also contains substances that inhibit the enzyme monoamine oxidase (MAO) which may also contribute to dependence from chronic use. Recall that MAO is the enzyme that breaks down monoamines such as dopamine; hence, Inhibiting MAO will result in greater levels of dopamine in the synapse.
In the periphery, nicotinic receptors are also found in autonomic ganglia and the neuromuscular junction of skeletal muscles. These receptors contribute to the functioning of sympathetic and parasympathetic nervous systems and voluntary motor movement.
Activation of nicotinic receptors can also produce negative effects such as gastrointestinal distress, irritation of the trachea, windpipe, and larynx, nausea and vomiting, and shortness of breath. This is especially true in individuals who are smoking for the first time.
At higher doses, nicotine produces a biphasic response, showing the effects of a depressant instead of a stimulant. This is due to how nicotine interacts with nicotinic receptors. After nicotine binds to the receptor, it becomes persistently depolarized and cannot be activated again for a short period, even if another agonist molecule binds to it during that time. With enough nicotine activity, receptors may spend most of the time depolarized. This is also referred to as depolarization blockade. The ion channels will be closed for longer than they are open, leading to functional antagonism.
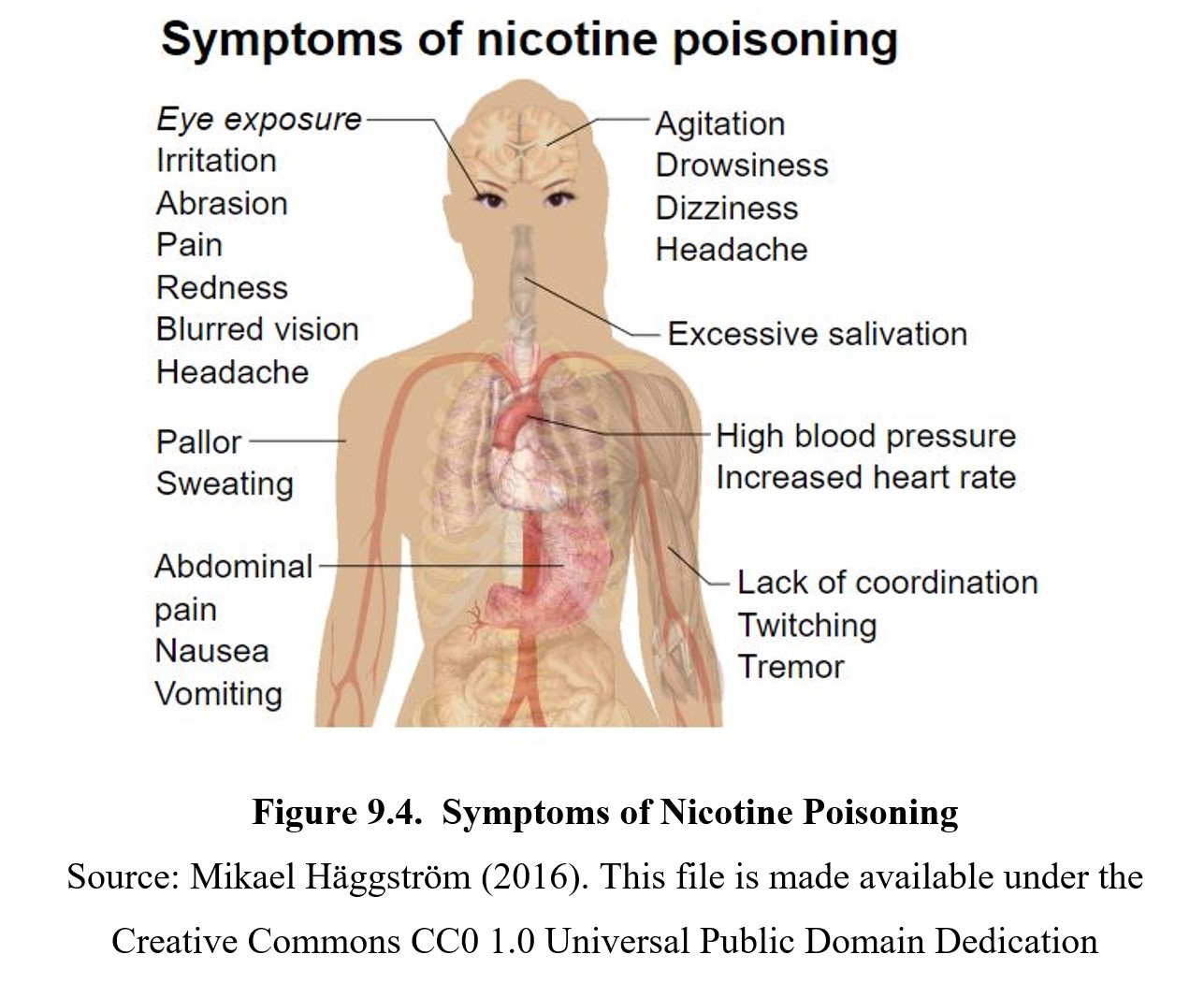
Nicotine is toxic at large doses. Initial symptoms include an increase in salivation, nausea, fluid in the lungs, high blood pressure, anxiety, muscle spasms, seizures, and an elevated heart rate (see the graphic below for a full list). This is eventually followed by low blood pressure and heart rate, difficulty breathing, and paralysis. In extreme cases, this can result in respiratory depression, heart failure, and death. During pregnancy, nicotine is toxic at lower doses and increases the risk of sudden infant death syndrome (SIDS) in breastfed infants.
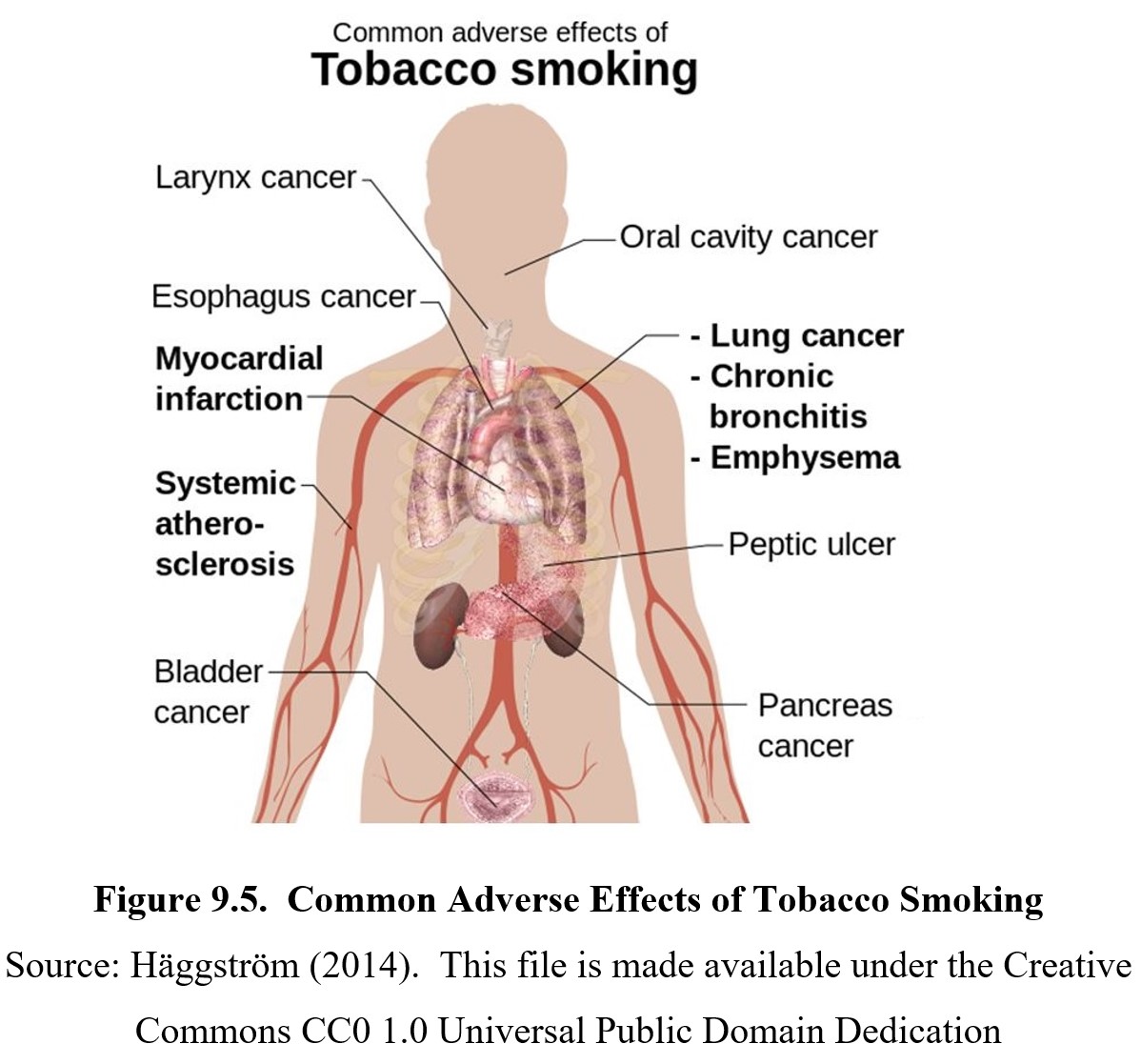
Some of the adverse effects associated with nicotine are the result of tobacco and smoking rather than the drug itself. Nicotine does not cause cancer, but smoke from tobacco contains over 4,000 chemicals, including 60 known carcinogens such as nitrosamines that can cause, initiate, or promote cancer. Smoking can also cause other pulmonary and cardiovascular diseases, as the particles are harmful to epithelial cells. Non-smokers can also be exposed to these risks through second-hand smoke. Major causes of fatalities due to cigarette smoking include heart disease, lung cancer, and chronic obstructive pulmonary disease (COPD).
9.1.4. Tobacco Use Disorder
The nicotine in tobacco is addictive, and chronic use can lead to tobacco use disorder. Nicotine can stimulate the neuronal release of dopamine and endogenous opioid peptides and activate the reward center of the brain. This causes a short-lasting but strong burst of euphoria, which creates a memory of this sensation and a desire to repeat the experience. In time, repetitive intake of nicotine leads to the development of tolerance and physical dependence.
Tolerance (neuroadaptation) is commonly attributed to the downregulation of nicotinic receptors in a compensatory response to overactivation to maintain homeostasis. Tolerance develops to some, but not all, effects of nicotine. The reduction of subjective effects of nicotine is attributed a pharmacodynamic rather than pharmacokinetic tolerance.
Development of tolerance to nicotine effects leads to increased smoking, which progresses to physical dependence and withdrawal when nicotine use is stopped. Withdrawal symptoms include a craving for nicotine or tobacco, increased irritability, anxiety, restlessness, difficulty concentrating, depression, headache, insomnia, and increased appetite. Although rarely life-threatening, these symptoms are unpleasant and explain why smoking can be so hard to quit. During withdrawal, nicotine use will relieve these symptoms and result in negative reinforcement, strengthening the habit.
Tobacco Addiction: Nicotine and Other Factors [4:54]
Treatment for nicotine addiction may involve nicotine replacement therapies. These allow users to gradually decrease nicotine use and avoid withdrawal symptoms while avoiding the health risks associated with smoking. Transdermal nicotine patches and nicotine-containing gums, lozenges, or nasal sprays are available. Certain drugs such as the antidepressant bupropion (Zyban®), the first non-nicotine-based drug for smoking cessation, can reduce cravings and mitigate the effects of withdrawal by acting at certain nicotinic receptors.
Successful treatment often involves one or more drug therapies in addition to behavioral therapies designed to help patients cope with temptations and deal with situations where smoking is habitual. Despite a large number of resources available for people who want to quit, relapse is still common. According to a 2015 survey, 70% of current adult smokers wished to quit, and 55% had attempted to do so in the past year. Only 7% were successful in quitting (CDC, 2017).
9.2. Caffeine
Section Learning Objectives
- Explain the history and uses of caffeine.
- Describe the pharmacokinetic properties of caffeine.
- Describe the pharmacodynamic properties of caffeine and explain the toxic effects of caffeine.
Although it is not likely to be thought of as a drug, caffeine is a stimulant compound that produces its psychoactive effects by targeting certain receptors in the nervous system, similar to every drug that we have discussed so far. Because we consider caffeine harmless and impose little-to-no regulation of it, caffeine is the most commonly used drug in the world.
9.2.1. Drug History and Overview
Caffeine is an alkaloid that is found in numerous plant species across the world. Some of the most notable sources of caffeine are the beans of coffee and cocoa plants, the leaves of tea plants, and kola nuts. Because of this, we can find caffeine in coffee, chocolate, tea, and many colas and other carbonated soft drinks. Today caffeine is the most popular stimulant in the world (nicotine is second). Theophylline is found mainly in tea, and theobromine occurs in larger proportions in cocoa.
Caffeine belongs to a class of stimulants called methylated xanthines, or methylxanthines for short. Methylxanthines share similar chemical structures derived from xanthine, a naturally occurring base found in many organisms, including humans. Other methylxanthines include theophylline and theobromine, which can be found in some of the same plants as caffeine. However, caffeine is the most common, so it will be the focus of this section.
The origins of caffeine consumption go back thousands of years. Caffeine has traditionally been consumed in various parts of the world, from tea in China, coffee in the Arabian Peninsula, and cocoa beans in the Americas. It is not known who first discovered the stimulant properties of caffeine, but it was first extracted in 1819 by the German chemist, Friedlieb Ferdinand Runge, who called it kaffebase (“coffee base”).
9.2.2. Administration and Pharmacokinetics
Caffeine is almost always administered orally in drinks, food, or pills. For beverages, the amount of caffeine administered depends on the drink, but it usually ranges from 10 to 200 mg per serving. See the table below for a list of examples:
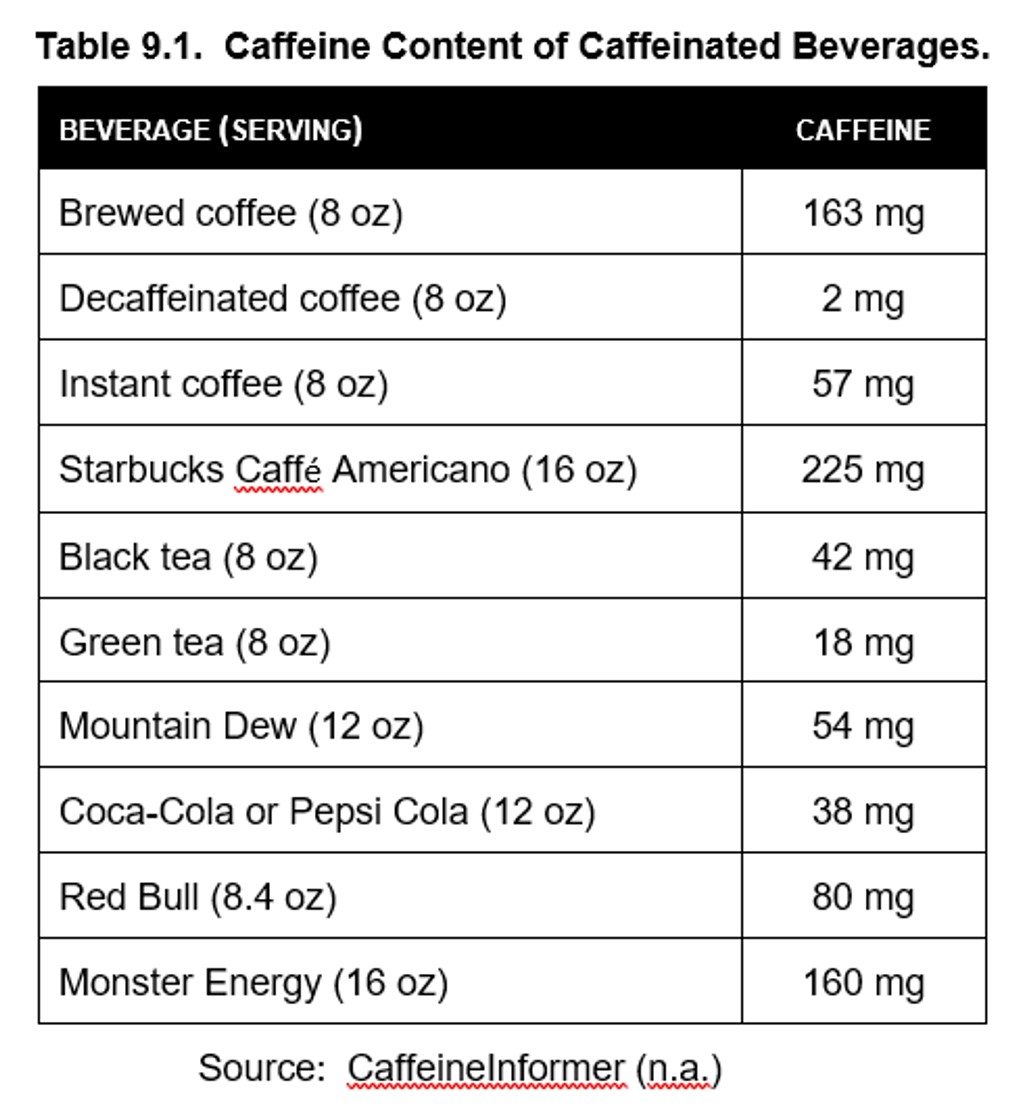
Caffeine is absorbed by the stomach and small intestine, with 99% being absorbed within 45 minutes of ingestion. Once absorbed, caffeine is quickly distributed throughout the body and can easily cross the blood-brain barrier. Blood concentration peaks between 30 to 120 minutes after ingestion, although effects are felt sooner-.
Cytochrome P450 enzymes in the liver, in particular CYP1A2, metabolize caffeine into primarily paraxantine as well as other methylxanthines such as theobromine and theophylline. Although they are active metabolites, they have much weaker effects than caffeine. Caffeine has a median half-life of about 5 hours, although this can vary among individuals, especially in the case of pregnant women in the last trimester, where the half-life can inexplicably increase to 18 hours. The cause of this extended half-life in pregnant women is uncertain, although CYP1A2 appears to be responsible for much of caffeine metabolism. The American College of Obstetricians and Gynecologists (ACOG) recommends that pregnant women should not consume more than 200 mg per day. Greater amounts of caffeine are associated with higher risk of loss of pregnancy and reduced fetal growth.
Caffeine has the potential to interact with a number of medications. Consuming caffeine while taking the nasal decongestant ephedrine carries a risk of hypertension, heart attack, stroke, and seizures. Caffeine can increase blood glucose levels and complicate the control of glucose levels in diabetic patients on oral hypoglycemic medications. Caffeine consumption by a patient on a serotonin medication such as a selective serotonin reuptake inhibitor (SSRI) can result in anxiety, confusion, restlessness, sleep disturbance, and other signs of serotonin syndrome (to be covered in Chapter 16).
9.2.3. Mechanisms of Action and Effects
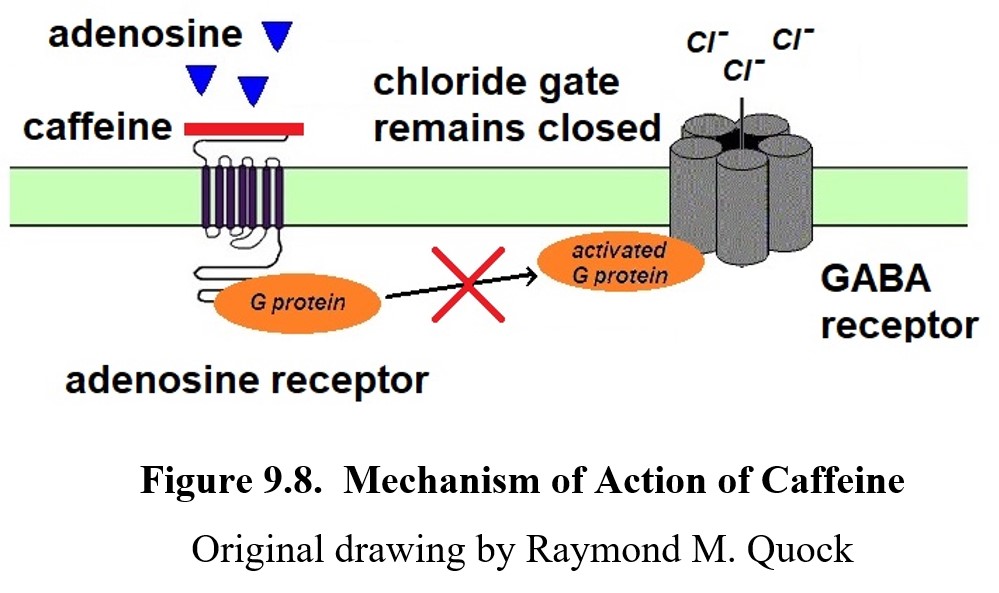
The primary mechanism of action for caffeine is the antagonism of adenosine receptors. Adenosine was not covered in our discussion of neurotransmitters in Unit 1, but it is a neuromodulator that is active throughout the nervous system. Following a long day of brain activity, there is an increase in the levels of adenosine, which is a breakdown product of adenosine triphosphate or ATP, the energy molecule that is found in all cells. Adenosine is taken up by neurons and glial cells. The adenosine from these sites produces an inhibitory effect in the ascending reticular activating system (ARAS), which determines the sleep/wake cycle. Current evidence posits adenosine as a positive modulator of GABA neurotransmission. By facilitating the inhibitory influence of GABA in the ARAS, adenosine inhibits the release of norepinephrine in the ARAS, contributing to sleep during the night. This is shown in the figure below.
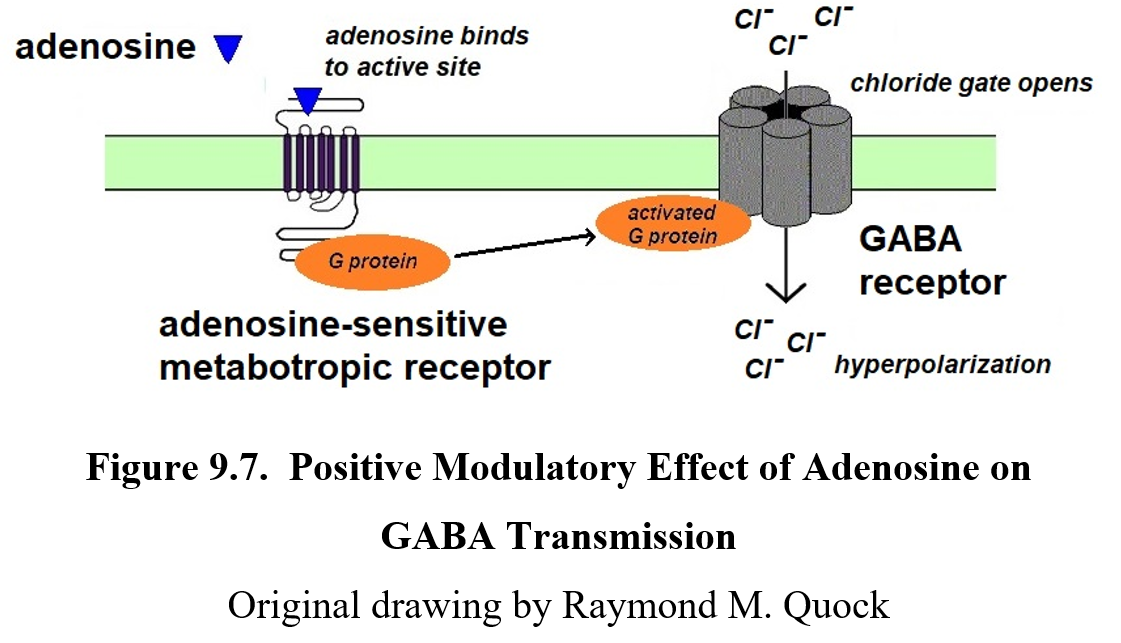
Caffeine possesses affinity for the adenosine receptor but lacks efficacy. By blocking adenosine receptors, caffeine negates the positive modulation and reduces the GABA inhibition on release of norepinephrine in the ARAS, and wakefulness and alertness are increased. Adenosine receptors also inhibit cholinergic and dopaminergic neurons, which helps explain why caffeine can cause jitteriness and dependence.
As a mild stimulant, caffeine can cause various physiological effects common to stimulants such as increased alertness and attention, improved mood, increased heart rate, and reduced appetite. Consumption of moderate amounts of caffeine is reported to reduce the risk of diabetes and cardiovascular disease. Negative effects of caffeine include anxiety, reduced control of fine motor movements, and increased blood pressure.
Caffeine Is a Psychoactive, But Is It Addictive? [4:37]
Chronic caffeine use can result in physical and psychological dependence. The DSM-V does not contain a specific diagnosis for caffeine use disorder but has recommended that it be studied further. Caffeine intoxication and caffeine withdrawal are recognized as disorders in DSM-V. Tolerance will develop to effects like increased alertness and improved mood. Therefore, withdrawal symptoms range from anxiety, fatigue, and irritability to depressed mood and difficulty concentrating. Headaches will often occur as the caffeine wears off due to the relaxation of blood vessels in the brain that were previously constricted by caffeine, resulting in a sudden increase in circulation.
Although rare, it is possible to overdose on caffeine, since large doses are toxic. Doses up to around 400 mg (approximately 3 cups of coffee, 10 cans of cola, or 2 energy drinks) are mostly harmless. Above this, caffeine can cause toxic effects such as anxiety, insomnia, irritability, and increased heart rate and blood pressure. This condition is known as caffeinism.
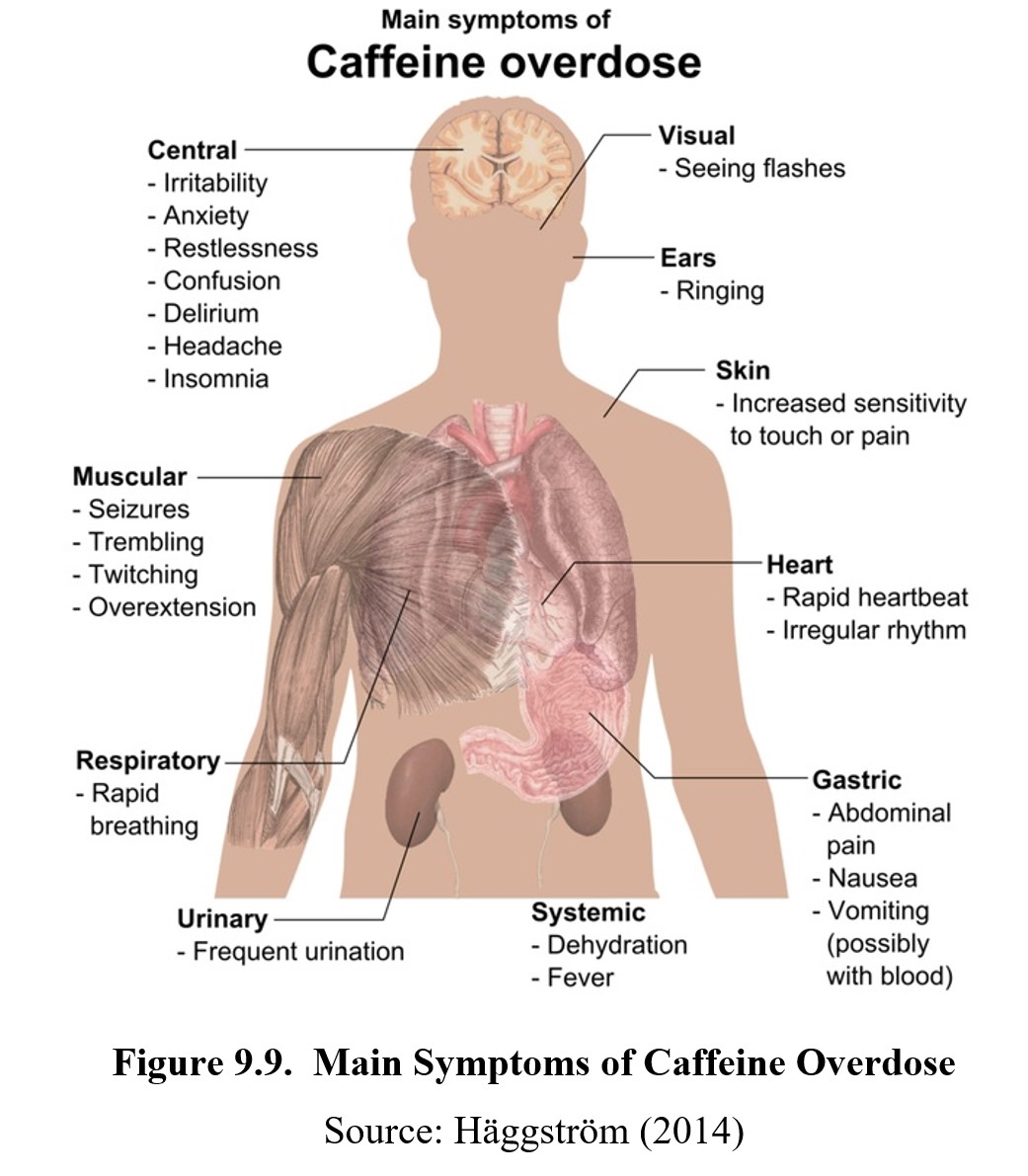
Fatal doses of caffeine are typically well beyond normal consumption levels for caffeinated beverages, and as such death from caffeine overdose is uncommon. However, there are bottles of caffeine powder sold as supplements that contain large amounts of pure caffeine. These can potentially lead to lethal doses if the user does not measure the correct amount. A teaspoon of pure caffeine powder is the equivalent of 25 cups of coffee. Following several fatalities from the consumption of pure caffeine powder in 2014, the FDA issued warnings about concentrated caffeine products and banned bulk sales of powders and liquids containing pure or concentrated caffeine.
Chapter Summary and Review
In this chapter, we finished up our coverage of stimulants by exploring the low-efficacy stimulants, nicotine, and caffeine. We compared different methods of administrating nicotine, then explained its mechanism of action and the consequences of chronic use. We also discussed caffeine’s role as the most commonly used drug, examining its effects on adenosine receptors and how caffeine dependence and overdose can occur.
Next chapter we will move on to the flip side of stimulants—depressants. With a new class of drugs, we will soon be learning about a different neuromodulator, GABA, and its function in the CNS as an inhibitor. Make sure that you are familiar with stimulants before moving on.
Chapter 9 Practice Questions
Answer the following questions:
- Is vaping a risk-free alternative to nicotine? Why or why not?
- Explain the following: firsthand smoke; secondhand smoke; and thirdhand smoke.
- Are nicotinic receptors ionotropic or metabotropic?
- Explain the widespread physiological and behavioral effects of nicotine.
- Name two specific mechanisms through which chronic smoking can lead to dependence.
- Name five symptoms of nicotine poisoning.
- Is nicotine tolerance pharmacokinetic or pharmacodynamic in nature?
- What are the signs of nicotine withdrawal?
- Is nicotine a carcinogen?
- What class of stimulants are caffeine and its active metabolites part of?
- What is the typical median half-life of caffeine?
- What is the relationship between caffeine and adenosine receptors?
- What is caffeinism? What are some of the symptoms of caffeinism?
- Out of all the stimulants discussed so far (cocaine, amphetamine, methamphetamine, nicotine, and caffeine), which drug is the most addictive? Which drug causes the most deaths? Which drug is used the most?
2nd edition
