Chapter 17: Anxiolytics
2nd edition as of August 2022
Chapter Overview
The next topics we will cover are anxiety disorders and anxiolytic drugs. Similar to depression, anxiety disorders are relatively common and can be treated with a combination of psychotherapy and anxiety-reducing drugs. In this chapter, we will study the biological basis of pathological anxiety and how anxiolytics such as benzodiazepines, buspirone, and SSRIs can compensate for the chemical imbalances in the brain responsible for it.
Chapter Outline
- 17.1.1. Types of Anxiety Disorders
- 17.1.2. Brain Regions Involved in Anxiety
- 17.1.3. Serotonin Hypothesis of Anxiety
- 17.2.1. Drug History and Overview
- 17.2.2. Administration and Pharmacokinetics
- 17.2.3. Mechanism of Action and Effects
- 17.3.1. Buspirone
- 17.3.2. SSRIs Revisited
- 17.3.3. Comparison of Anxiolytic Drugs
Chapter Learning Outcomes
- Outline types of anxiety disorders, prevalence of, and causes.
- List and describe types of anxiolytic drugs.
17.1. Overview of Anxiety
Section Learning Objectives
- Describe anxiety disorder and its prevalence and subtypes.
- Explain which brain regions are involved in anxiety.
- Explain the neurochemical basis of anxiety.
We have all been anxious before. While watching a scary movie, we might feel our heart race and muscles tense up, or experience shortness of breath and sweaty palms. In anticipation of a big exam, we may start to feel restless and worry about failing. These are the characteristics of regular, everyday anxiety that we all experience.
But similar to how depression is distinct from normal sadness, anxiety disorders are a more severe form of anxiety that interferes with daily life. In these cases, the feeling of anxiety is so extreme or persistent that the people suffering from it are unable to escape. We will begin this chapter by examining the different types of anxiety disorders and how anxiety is represented in the brain.
17.1.1. Types of Anxiety Disorders
As mentioned at the start of the chapter, anxiety disorders are common. They are the most common mental illness in the U.S., although they are highly treatable. Less than 40% of those with anxiety disorders received treatment.
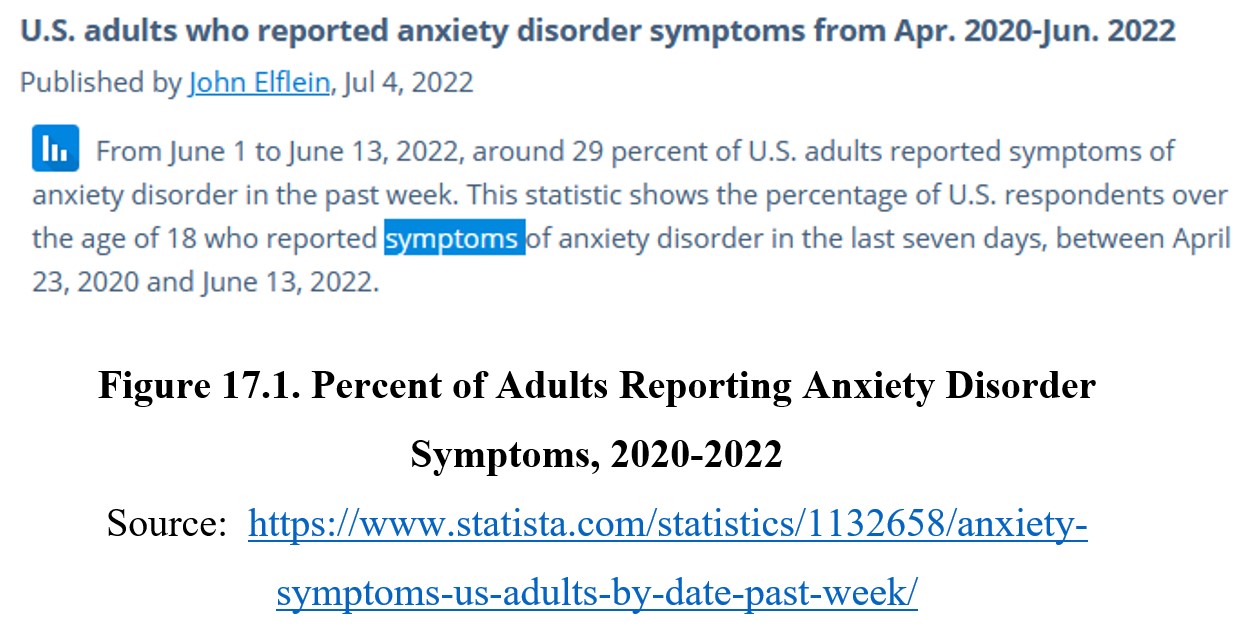
The prevalence of U.S. adults reporting anxiety disorder was around 19.1%. As you can see, the prevalence increased from 19.1% to 29.0% over a two-year period. This no doubt reflects the impact of the COVID-19 pandemic on mental health. Women are more likely to experience anxiety disorders than men, possibly due to differences in hormones and brain chemistry. Although they can occur at any age, anxiety disorders are most common in middle-aged adults, 30-44 years of age. According to the NIH, nearly a third of all adolescents 13-18 years in age, have experienced an anxiety disorder.
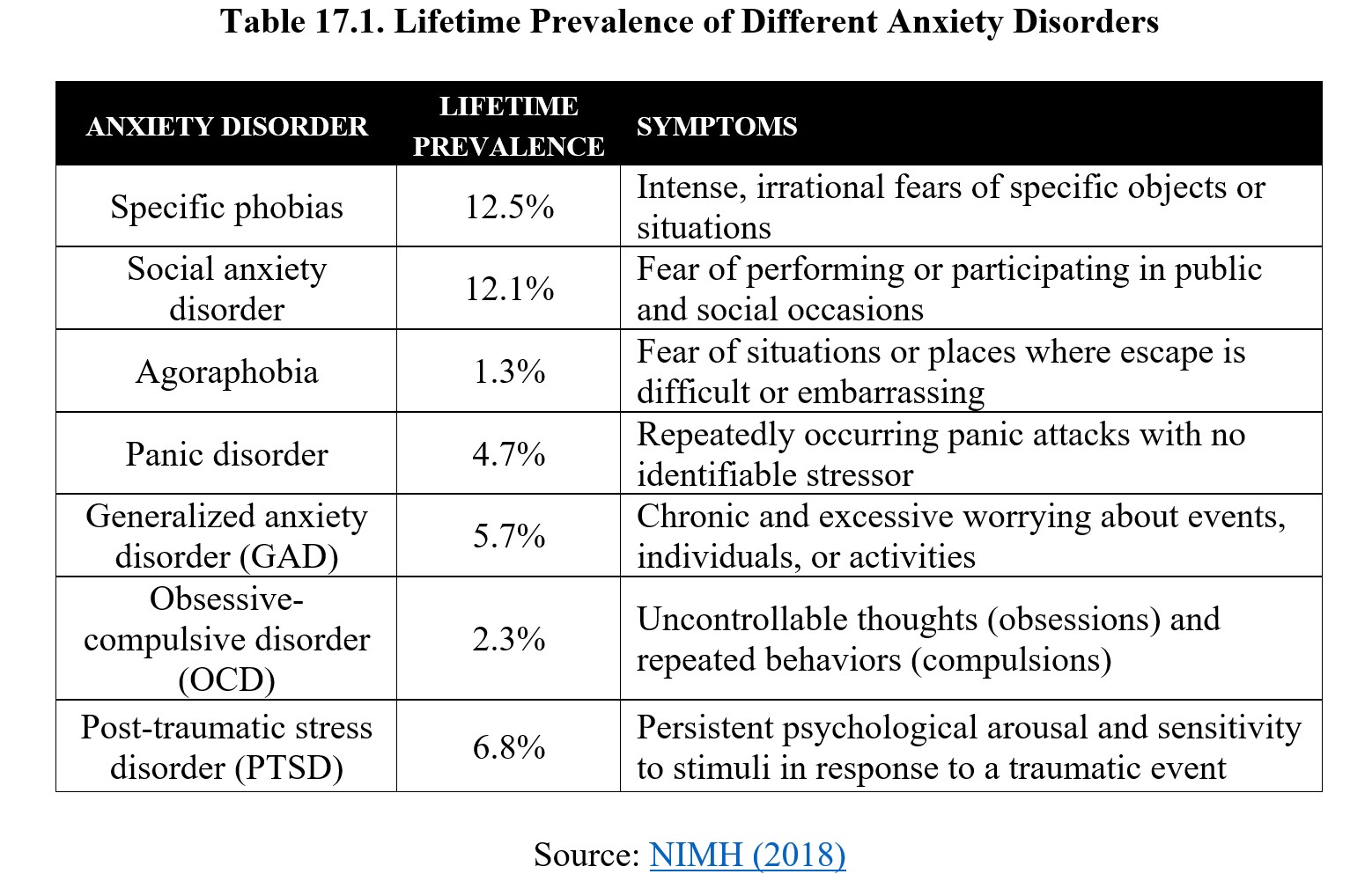
There are many different types of anxiety disorders. The most common are specific phobias, which are intense fears or anxieties that arise from specific objects or situations that pose little or no actual danger. Note that this is not the same as simply disliking something. People with phobias will go to extreme lengths to avoid the things they are afraid of, to the point where their daily life is impaired. If you are interested, the site below has a list of some of the most common phobias (you do not need to know them for this class):
Also common is social anxiety disorder. This is a persistent fear of performing or participating in public or social occasions. These situations cause intense and immediate anxiety that can be severe enough to cause a panic attack. A related (but distinct) phobia is agoraphobia. People with agoraphobia are afraid of situations where escape is difficult or embarrassing. People with agoraphobia are more likely to avoid social situations entirely, while those with social anxiety disorder do not experience anxiety unless attention is turned towards them.
All types of anxiety disorders can cause panic attacks. These are episodes of intense fear accompanied by physical symptoms that may resemble a heart attack, such as chest pain, shortness of breath, and dizziness. If panic attacks occur repeatedly and without obvious causes, it becomes classified as a panic disorder. People with panic disorder may mistakenly believe that they are suffering from some sort of chronic ailment, rather than a psychological disorder.
Some people feel anxious all of the time. Chronic and excessive worrying may qualify as generalized anxiety disorder (GAD), which may be associated with symptoms such as high blood pressure and rapid breathing. People with GAD may feel exhausted all the time because of the constant stress.
There are two other anxiety disorders that you have no doubt heard of. The first is obsessive-compulsive disorder (OCD), which consists of uncontrollable thoughts (obsessions) that lead to repeated behaviors (compulsions). Again, this is more severe than simply being particular or having the desire to keep things neat. People with OCD may spend hours before leaving the house triple- and quadruple-checking that all of the appliances and devices are unplugged or washing their hands repeatedly to the point where the skin becomes raw.
Finally, you have also probably heard of post-traumatic stress disorder (PTSD). PTSD may develop in response to traumatic events such as combat, natural disasters, or sexual assault. It is characterized by a persistent state of physiological arousal and an exaggerated response to stimuli. People with PTSD may experience vivid flashbacks or dreams where they relive the traumatic experience, suffer from sleep disruption, and feel numb or detached from their surroundings.
These illnesses make up the majority of anxiety disorders. Below is a table summarizing the different types:
17.1.2. Brain Regions Involved in Anxiety
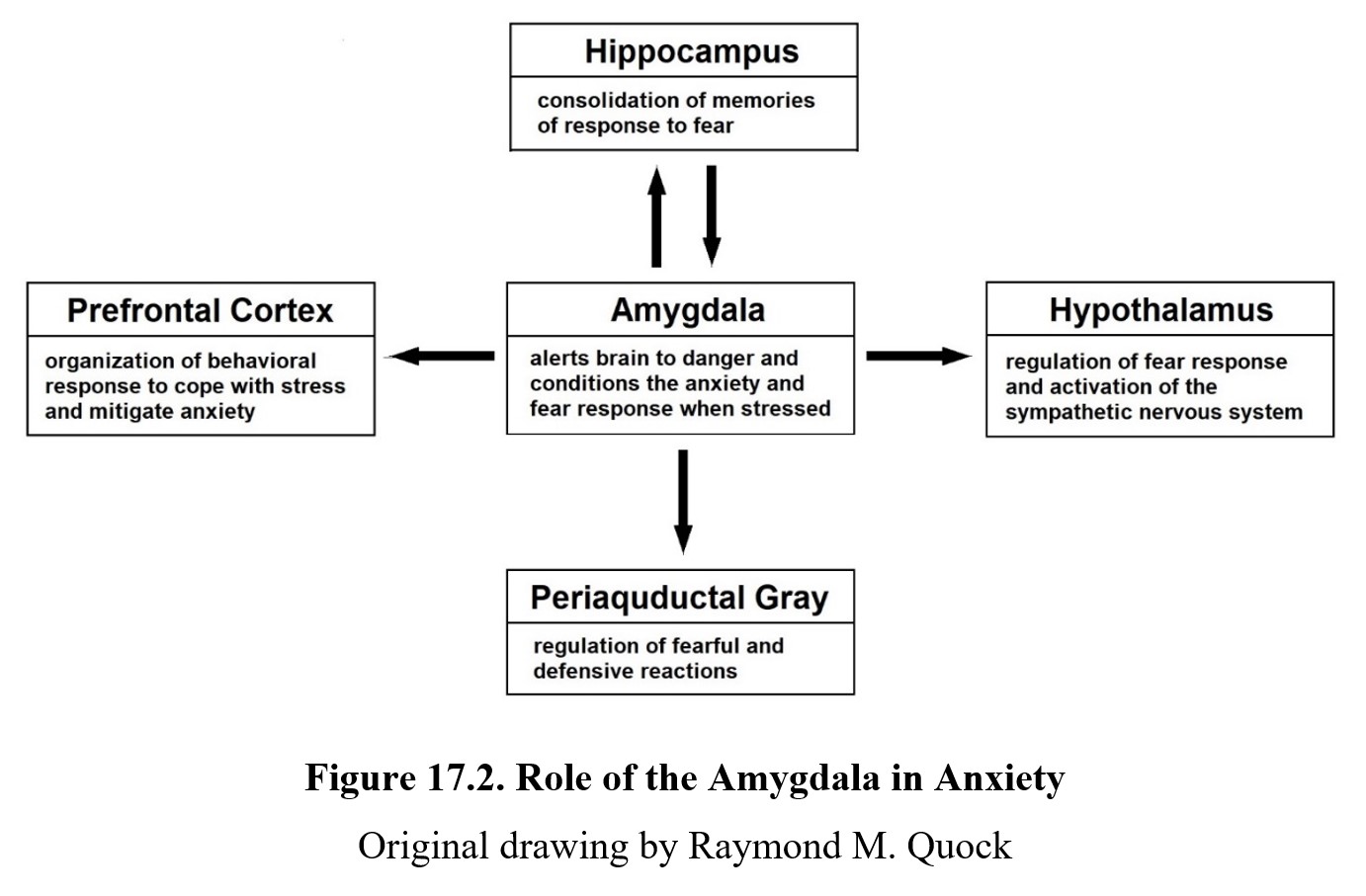
What areas of the brain are responsible for anxiety? Although the processes related to anxiety are distributed throughout the brain, some regions play a larger role than others. Perhaps the most significant area related to anxiety is the amygdala. We described this region back in Chapter 2 as being associated with emotional responses like fear and aggression. We also defined the hippocampus and its role in storing memories. Both structures are part of the limbic system, a part of the forebrain that influences motivation and emotions.
It should come as no surprise that the amygdala is involved in anxiety disorders, given how fear is a central component of anxiety. Indeed, the amygdala is responsible for processing the relationship between a fear-inducing stimulus and our response. The amygdala works with the hippocampus, which encodes contextual information about the stimulus, to form a conditioned (i.e., learned) fear response.
In anxiety disorders, the amygdala may be overactive. Studies have shown that amygdala activity is increased in patients with any type of anxiety disorder. This persistent and unnecessary activation can lead to other disorders or issues. For instance, chronic stress may lead to damage to the hippocampus and memory impairment similar to depression.
The amygdala sends information about fear-related stimuli to many different parts of the brain. Signals sent to the prefrontal cortex initiate a behavioral response to threats. The periaqueductal grey (PAG), which you may remember from the chapter on opioids, activates the endogenous opioid system to provide pain relief in expectation of danger, as well as increased feelings of dread. The amygdala also communicates with the hypothalamus to initiate the fight-or-flight response through the sympathetic nervous system.
To summarize, the overactivity of the amygdala is linked with anxiety disorders. The amygdala itself communicates with many different structures to create a conditioned fear response, which can then be triggered again by similar stimuli in the future. Below is a diagram summarizing the main structures involved:
17.1.3. Serotonin Hypothesis of Anxiety
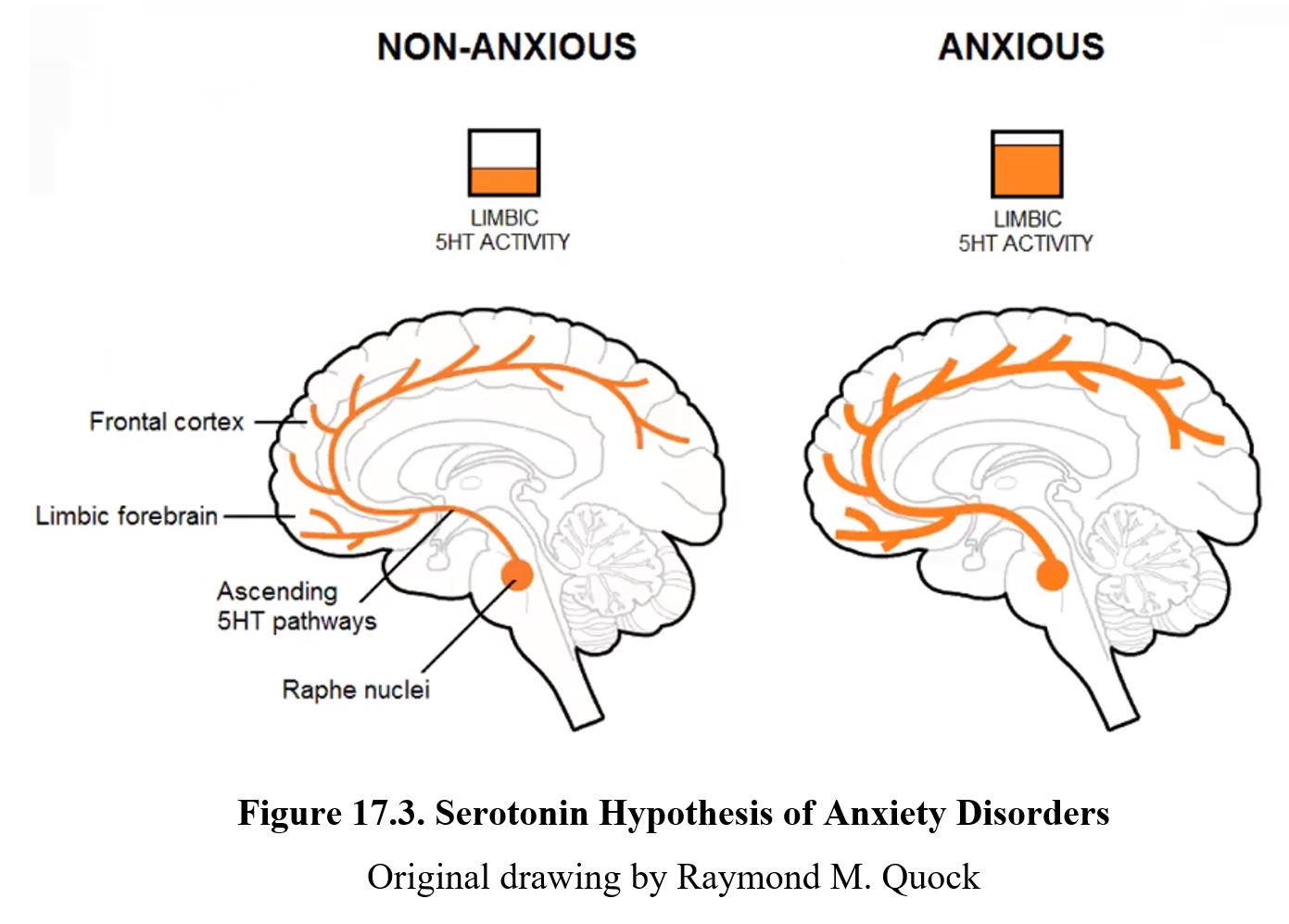
Now that we know what structures are involved in anxiety, what role does neurotransmission play in anxiety disorders? As is the case with depression, although the exact mechanisms are not known, it is hypothesized that a chemical imbalance in neurotransmitter activity is partly responsible. This idea is known as the serotonin hypothesis of anxiety since serotonin is the primary neurotransmitter implicated in anxiety disorders.
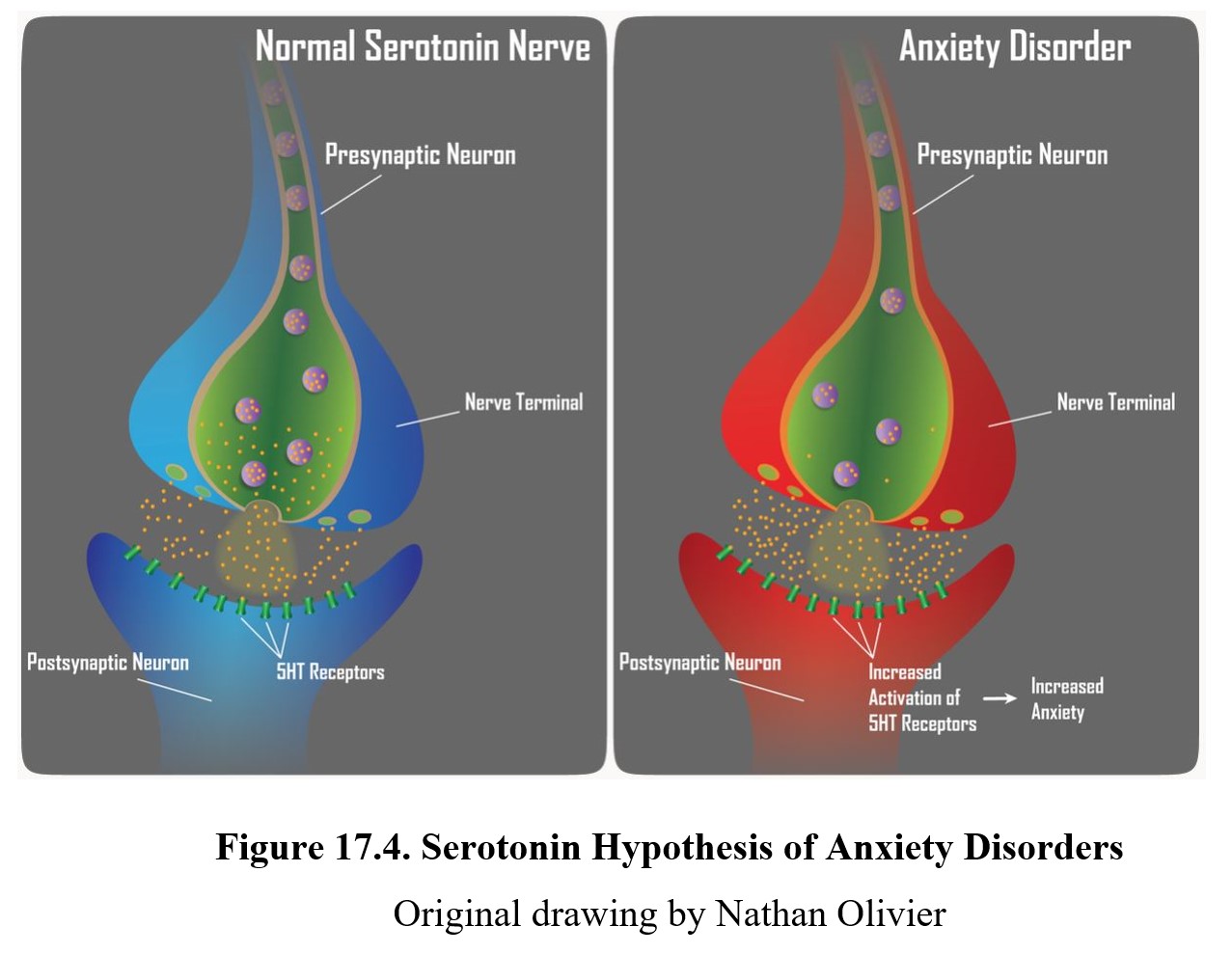
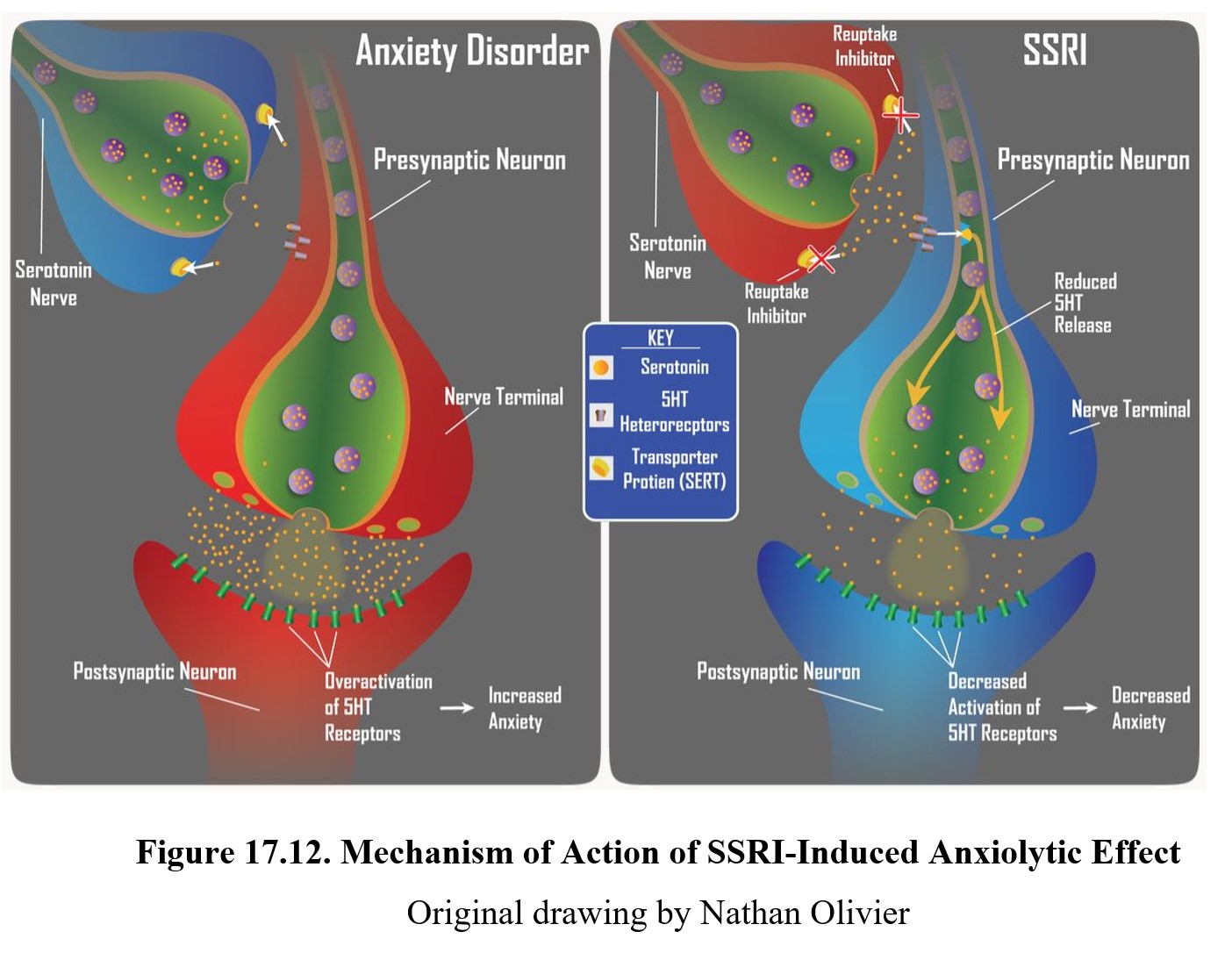
Recall how depression may be caused by low levels of norepinephrine and serotonin activity in the limbic system. Anxiety is thought to be connected to high levels of serotonin instead. Below is a diagram demonstrating this. A large cluster of serotonergic neurons can be found in the raphe nuclei, a part of the midbrain. These neurons project to other parts of the limbic system and the cortex through ascending serotonin pathways. In non-anxious people, these pathways have a normal level of activity. Yet, in people with anxiety disorders, these pathways are overactive.
Serotonin & Anxiety: Raphe Nucleus [1:15]
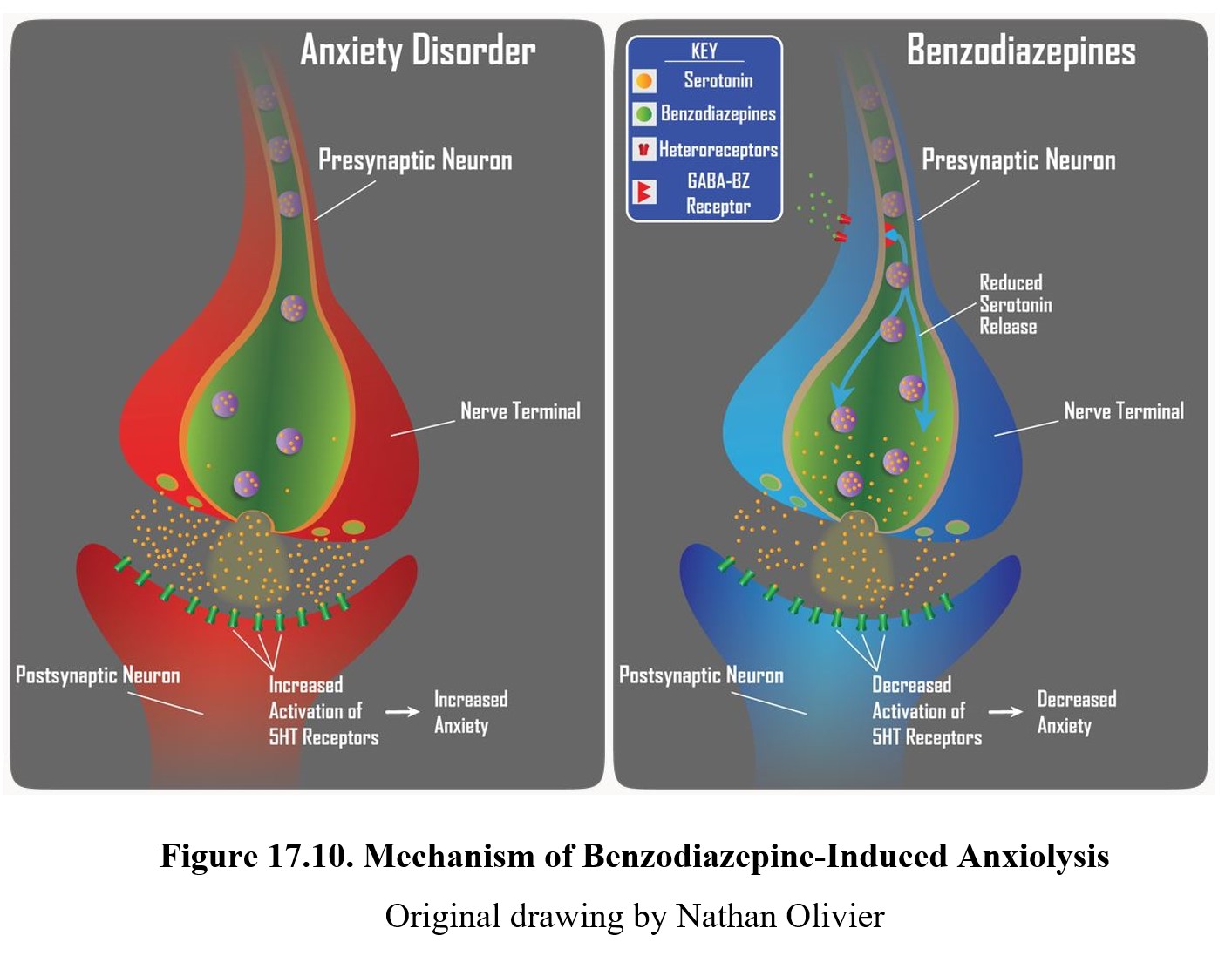
Below you can see another representation of this idea, this time at the level of the synapse. The serotonergic neurons release transmitter into the synapse, where they then activate 5-HT receptors on the postsynaptic neuron (left panel above and upper panel below). Overactivation of these 5-HT receptors is thought to be linked with increased levels of anxiety (right panel above and lower panel below).
17.2. Benzodiazepines
Section Learning Objectives
- Explain the history of benzodiazepines and define nonbenzodiazepines or Z-drugs.
- Describe the pharmacokinetic properties of benzodiazepines.
- Describe the pharmacodynamic properties and effects of benzodiazepines.
With our understanding of how anxiety works in the brain, we now turn our attention to anxiolytic drugs. An anxiolytic is a drug that can reduce anxiety. Our first example is benzodiazepines. These were once the most commonly prescribed medications in the 1970s, although they have been somewhat replaced by newer drugs.
17.2.1. Drug History and Overview
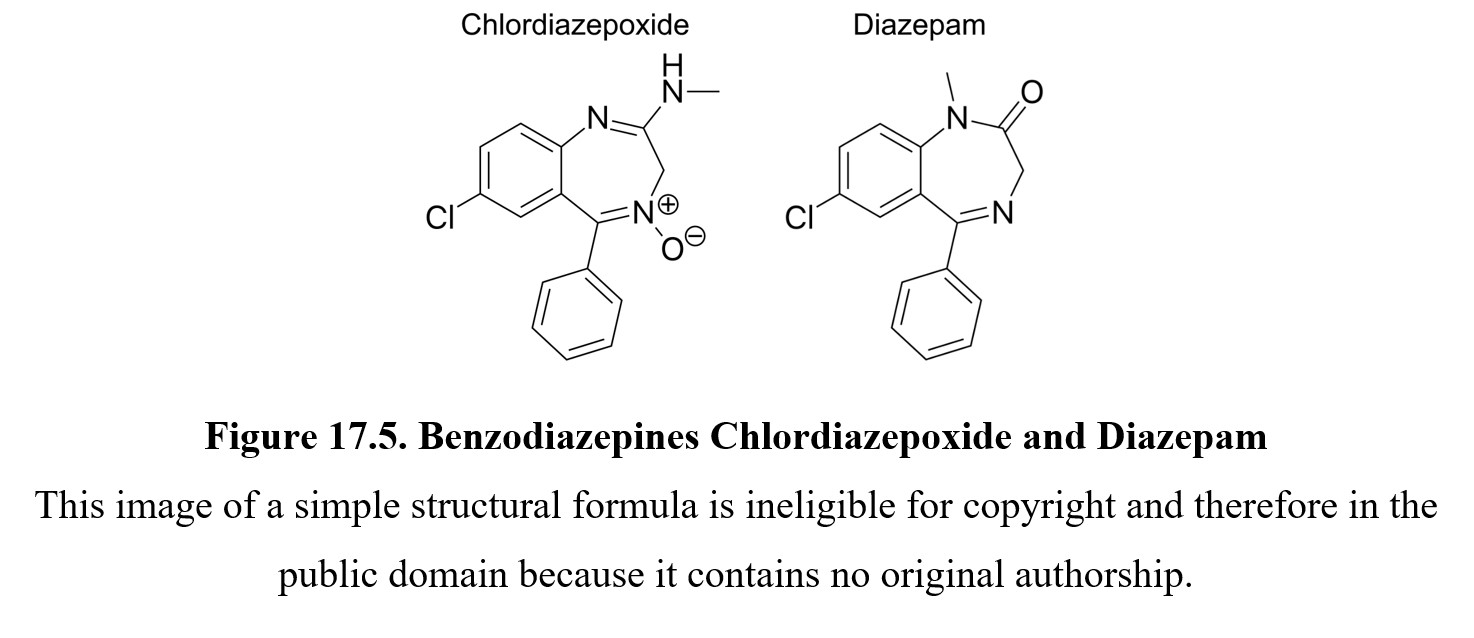
Benzodiazepines were first discovered in 1955 by a chemist at Hoffmann-La Roche working on the development of new tranquilizers. The substance, chlordiazepoxide, was found to have strong sedative effects and was soon after marketed under the brand name Libirum®. Soon after, Hoffmann-La Roche developed diazepam, another benzodiazepine, and began selling it under the name Valium®. The name benzodiazepine comes from the main chemical feature of these drugs, linked benzene and diazepine rings, as seen below.
Similar to barbiturates, benzodiazepines are typically classified by their duration of action. An ultrashort-acting benzodiazepine is midazolam (Versed®) which is used as an i.v. anesthetic or preanesthetic medication prior to surgery. Short-acting drugs such as alprazolam (Xanax®) or lorazepam (Ativan®) are used to treat anxiety disorders, panic disorders, and insomnia, among other uses. Long-acting benzodiazepines include the original chlordiazepoxide (Librium® and diazepam (Valium®) used to treat chronic anxiety disorders and to relieve alcohol withdrawal.
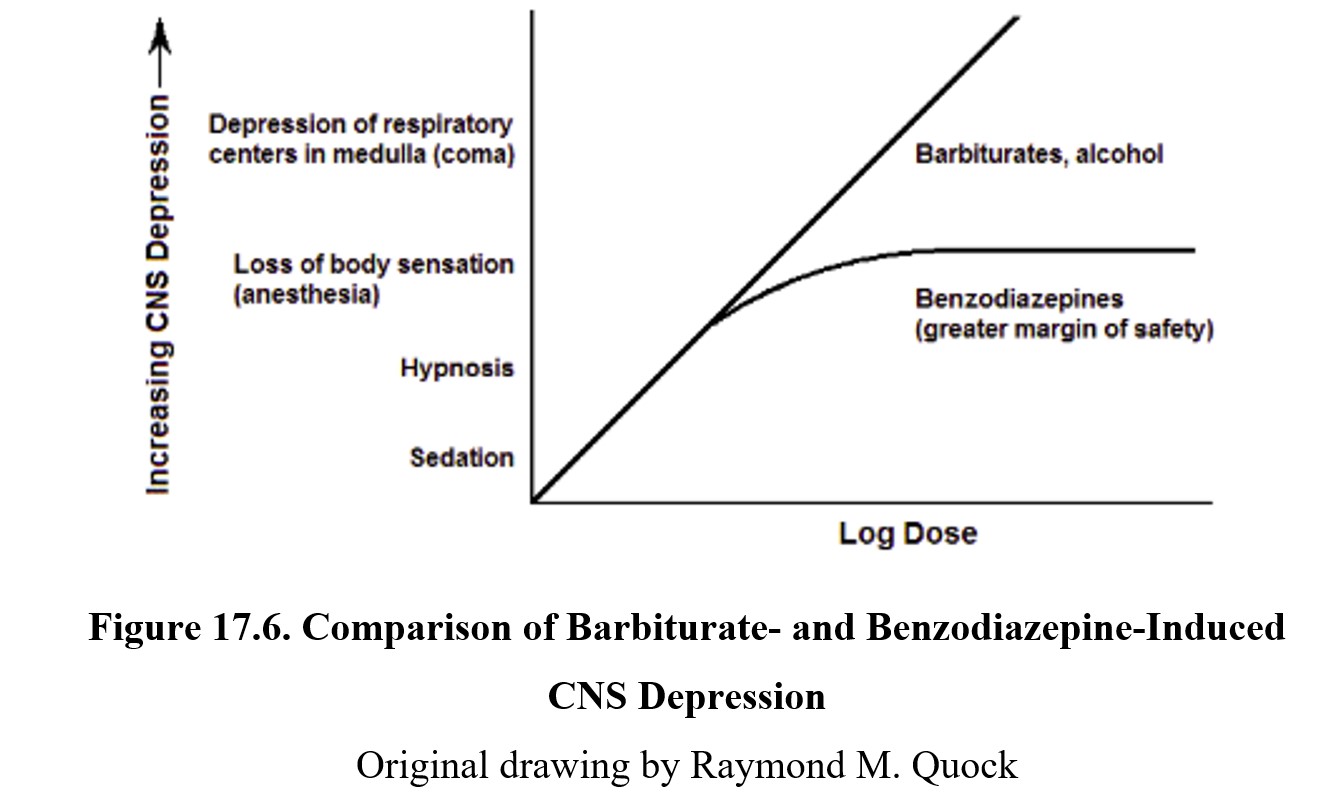
Benzodiazepines quickly replaced barbiturates (which we covered in the chapter on CNS depressants) as the preferred sedative-hypnotic drugs because they showed improved drug safety. Benzodiazepines have a lower ceiling effect than barbiturates. At therapeutic doses, benzodiazepines entirely lack the respiratory depressant effects of barbiturates, which contributed to the risk of a fatal overdose (see below).
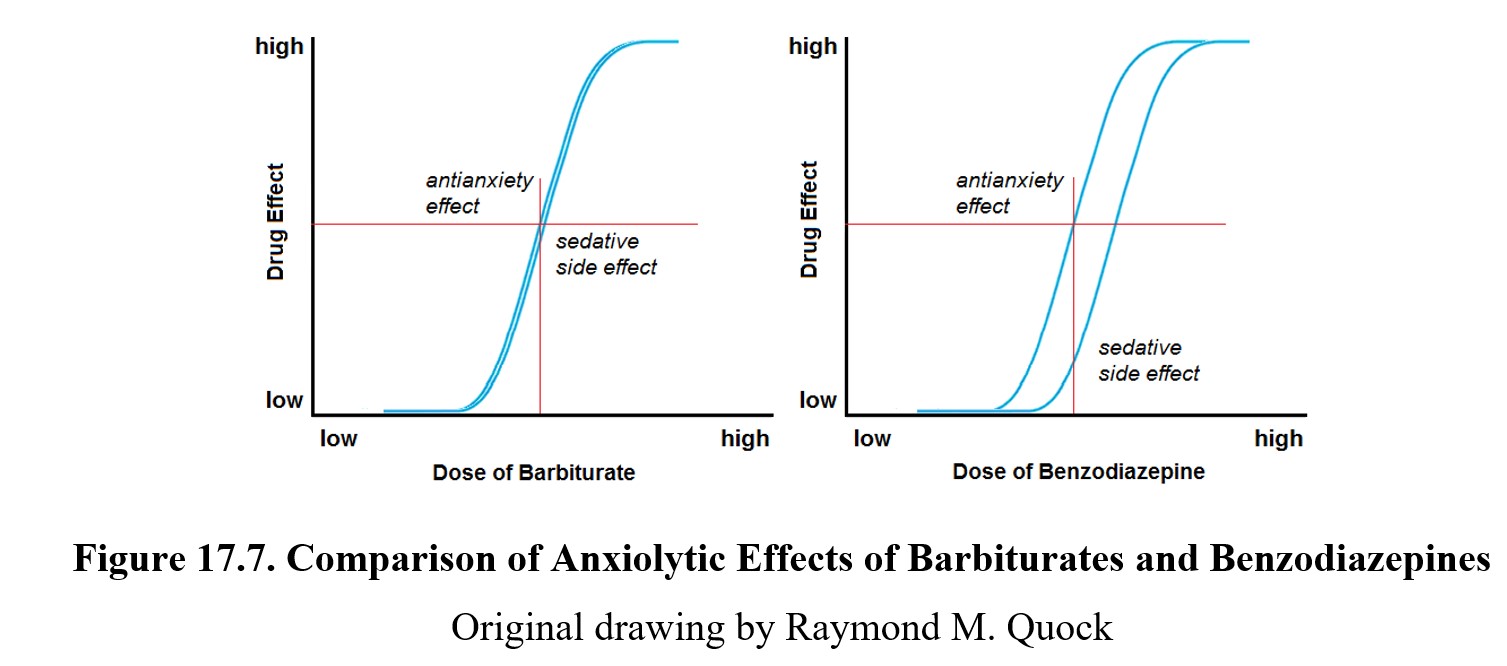
Benzodiazepines also replaced barbiturates for antianxiety use. Ideally, an anxiolytic should be able to provide an antianxiety effect without producing significant sedative side effects. This was part of the issue with barbiturates. Benzodiazepines were an improvement because, at doses that would produce the same antianxiety effect, benzodiazepines produced less sedative side effects compared to barbiturates, as seen in the graphs below:
By the 1970s, benzodiazepines were widely used for many different. More benzodiazepines were developed, such as alprazolam (Xanax®) and lorazepam (Ativan®). In fact, they were for a time the most commonly prescribed medications in the world. As time went on, however, studies began to indicate that benzodiazepines did produce dependence, and that many patients met the criteria for benzodiazepine dependence. This slowed the rate of prescriptions and brought concerns to the forefront.
Although benzodiazepines are still prescribed to treat anxiety, they have largely been replaced as sedative-hypnotics by non-benzodiazepines. Despite the name, these drugs are similar to benzodiazepines in terms of effects. They are referred to as non-benzodiazepines because they lack the benzene-diazepine structure. For reasons we will discuss later, these drugs have powerful sedative-hypnotic effects but lack antianxiety effects. They are also known as Z-drugs because many of them such as zolpidem (Ambien®) or zaleplon (Sonata®) begin with the letter Z.
17.2.2. Pharmacokinetics
Benzodiazepines are typically taken orally, although they can be injected IV or IM or administered rectally. The most important pharmacokinetic property of benzodiazepines is their half-lives. Some benzodiazepines have very short (1–12 hours) half-lives, while others have very long (40+ hours) half-lives.
A hypnotic benzodiazepine with a short half-life tends to be rapidly converted into inactive metabolites. These drugs are more suitable for treating insomnia due to the onset and duration of effect, although as mentioned earlier, they have largely been replaced by Z-drugs.
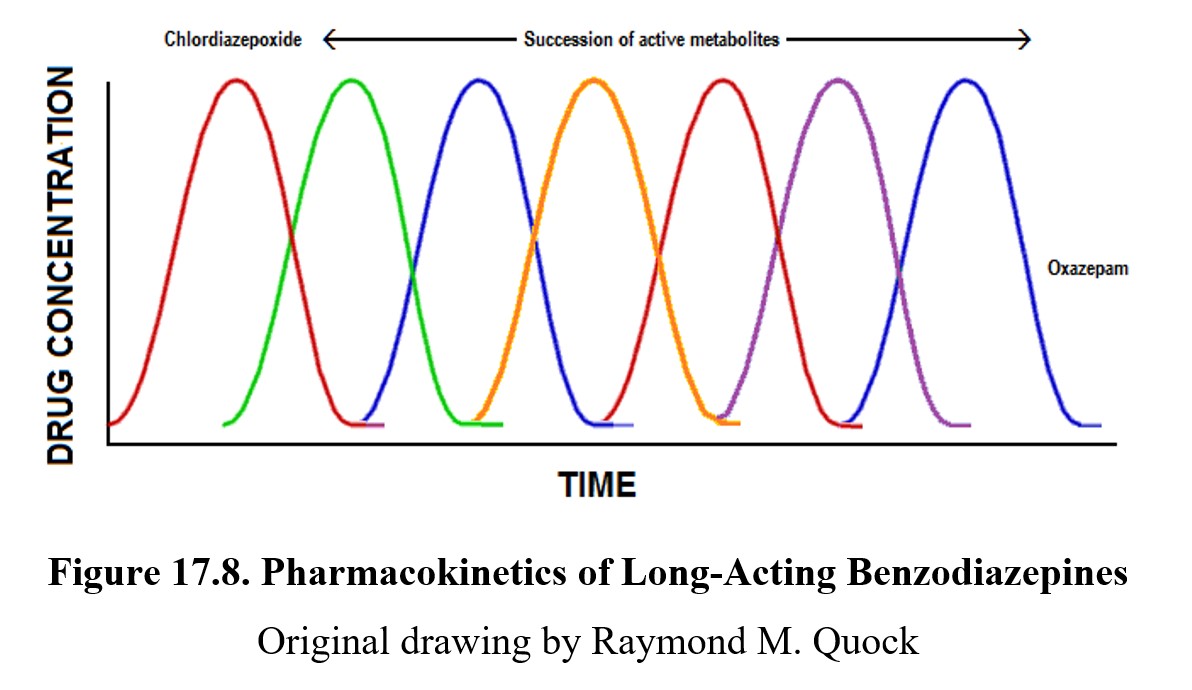
In comparison, long-acting benzodiazepines have extended half-lives because they are metabolized into a succession of active metabolites (see below). For example, following the administration of chlordiazepoxide, the amount of the actual drug peaks and then drops. The chlordiazepoxide is converted to an active metabolite, which altered to another active byproduct, which is changed into yet another active metabolite, so on and so forth, until a more easily byproduct (oxazepam) is produced. This is why the actual sojourn of the parent compound (chlordiazepoxide) is short compared to the duration of its effects. This prolongs the duration of effect considerably and makes long-acting benzodiazepines more effective in treating chronic anxiety conditions. They are also preferred because they have less severe withdrawal symptoms because blood levels of the drug decline very slowly.
Although benzodiazepines are relatively safe when taken as directed and are unable to trigger respiratory depression on their own, they can be deadly when taken with other CNS depressants such as alcohol, Z-drugs, or other benzodiazepines. The drug interactions of multiple CNS depressants can be synergistic, meaning the overall effect is greater than when simply adding the expected effects together.
In some cases, this can be the goal of misuse. Benzodiazepines used recreationally tend to be taken with other drugs to enhance their effects in some way. One example is taking short-acting benzodiazepines with alcohol, which increases the buzz while allowing the user to drink fewer calories. Although recreational use does occur, it is relatively infrequent; most misuse starts with patients who were originally prescribed benzodiazepines and develop dependence and addiction.
17.2.3. Mechanism of Action and Effects
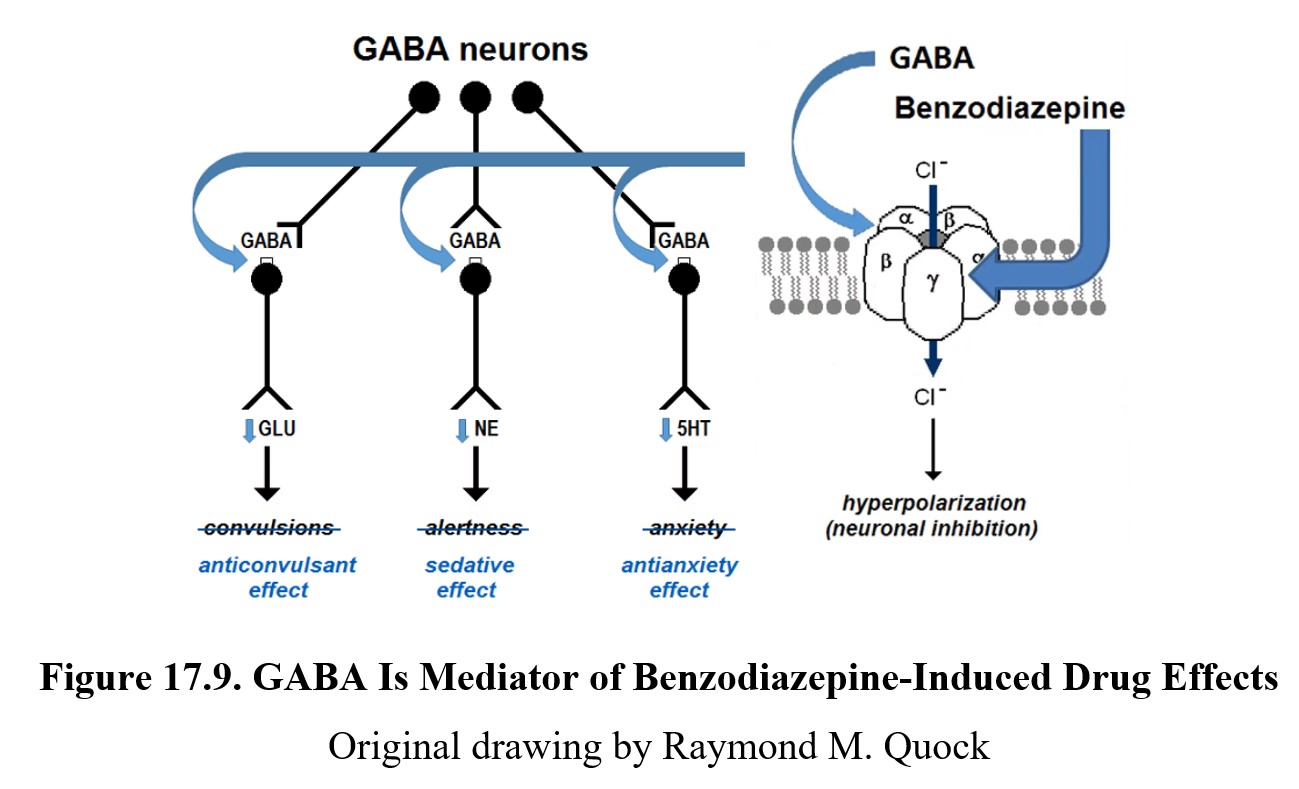
Knowing that benzodiazepines are sedative-hypnotics, it should come as no surprise that their primary mechanism of action is at the GABA receptor. More specifically, they interact with the GABAA receptor. GABAA, if you’ll recall, is an ionotropic receptor that is part of the GABAA chloride channel receptor complex. When the channel is opened, it allows an influx of chloride ions into the cell. This hyperpolarizes the neuron, leading to inhibition of neural activity.
Benzodiazepines are positive allosteric modulators of the GABAA receptor. Recall that an allosteric modulator is a ligand that binds to a site other than the primary site and changes how that site functions. This means that benzodiazepines do not directly activate the GABAA receptor. Instead, they enhance the sensitivity of the GABAA receptor for the transmitter. This makes it easier for lower levels of GABA to activate the receptor.
GABA is the main inhibitory neurotransmitter in the brain and is responsible for the inhibition of many other transmitters, including glutamate, norepinephrine, and serotonin. By increasing GABA signaling, benzodiazepines can decrease the activity of these transmitters. As you can see in the image below, this causes a variety of effects. Inhibition of glutamate transmission receptors produces an anticonvulsant effect, while inhibition of norepinephrine transmission induces a sedative effect.
For the use of benzodiazepines as an anxiolytic, we are mostly concerned with the effect they have on serotonin transmission. Consult the image below. Inhibitory GABA neurons synapse with the presynaptic neuron. In cases of anxiety, this neuron is overactive, releasing large amounts of serotonin into the synapse. Benzodiazepines bind to heteroreceptors on the presynaptic neuron, enhancing the inhibitory effects of GABA on the neuron. This reduces the release of serotonin, as shown in the lower panel of the figure below and causes the anxiolytic effect.
Benzodiazepines cause other side effects associated with their widespread effect on GABA inhibition. One side effect is anterograde amnesia. Benzodiazepines also impair certain cognitive functions such as reaction time and visual-spatial ability, which can cause issues with complex tasks such as driving. People tested a day after taking benzodiazepines showed reduced driving skills similar to people with a blood alcohol concentration of 0.05–0.10%.
Although we have been talking about GABAA receptors as if they are all identical, there are actually many different subtypes based on the identities of the protein subunits that make up the chloride channel. Benzodiazepines interact with these subtypes differently. Some GABAA receptors have a benzodiazepine binding site known as a BZ1 receptor, while others have a BZ2 receptor. There are also GABA receptors that may lack a BZ binding site entirely.
Activation of BZ1 and BZ2 receptors produces different effects. BZ1 is responsible for the sedative-hypnotic and anticonvulsant effects, while BZ2 mediates anxiety relief and impairment of cognitive functions. Most benzodiazepines act at both BZ receptors, but many Z-drugs, such as zolpidem (Ambien®), zaleplon (Sonata®), and eszopiclone (Lunesta®), are selective for the BZ1 receptor. This is why Z-drugs produce sedative-hypnotic effects but not anxiolytic effects.
As mentioned previously, tolerance and dependence on benzodiazepines can occur, especially with misuse of these drugs. Tolerance builds to the sedative and anticonvulsant effects of the drug, but not to amnesia and cognitive impairment. Abrupt discontinuation of benzodiazepines can result in rebound effects (e.g., insomnia returning worse than before) and withdrawal symptoms. Benzodiazepine withdrawal is similar to alcohol withdrawal and can produce severe symptoms such as seizures and delirium tremens. As mentioned previously, short-acting benzodiazepines tend to have more frequent and severe withdrawal signs compared to long-acting benzodiazepines.
17.3. Other Anxiolytic Drugs
Section Learning Objectives
- Explain the mechanism of action of buspirone.
- Explain how SSRI antidepressants might be effective in reducing anxiety.
- Describe the recommended pharmacotherapies for different anxiety disorders.
Although benzodiazepines are still prescribed for anxiety, their use is not ideal because of the dependency and withdrawal mentioned above. Fortunately, in recent decades, other anxiolytic drugs with fewer adverse effects have been identified. We will cover a few of them in this section before comparing their applications to different anxiety disorders.
17.3.1. Buspirone
The first drug that we will examine is buspirone. It is a novel non-benzodiazepine and partial agonist of 5-HT1A receptors. These are presynaptic autoreceptors that, when activated, inhibit the release of serotonin. By binding to these receptors, buspirone is capable of decreasing the amount of serotonin in the synapse, thus reducing the activation of postsynaptic serotonin receptors (see below).
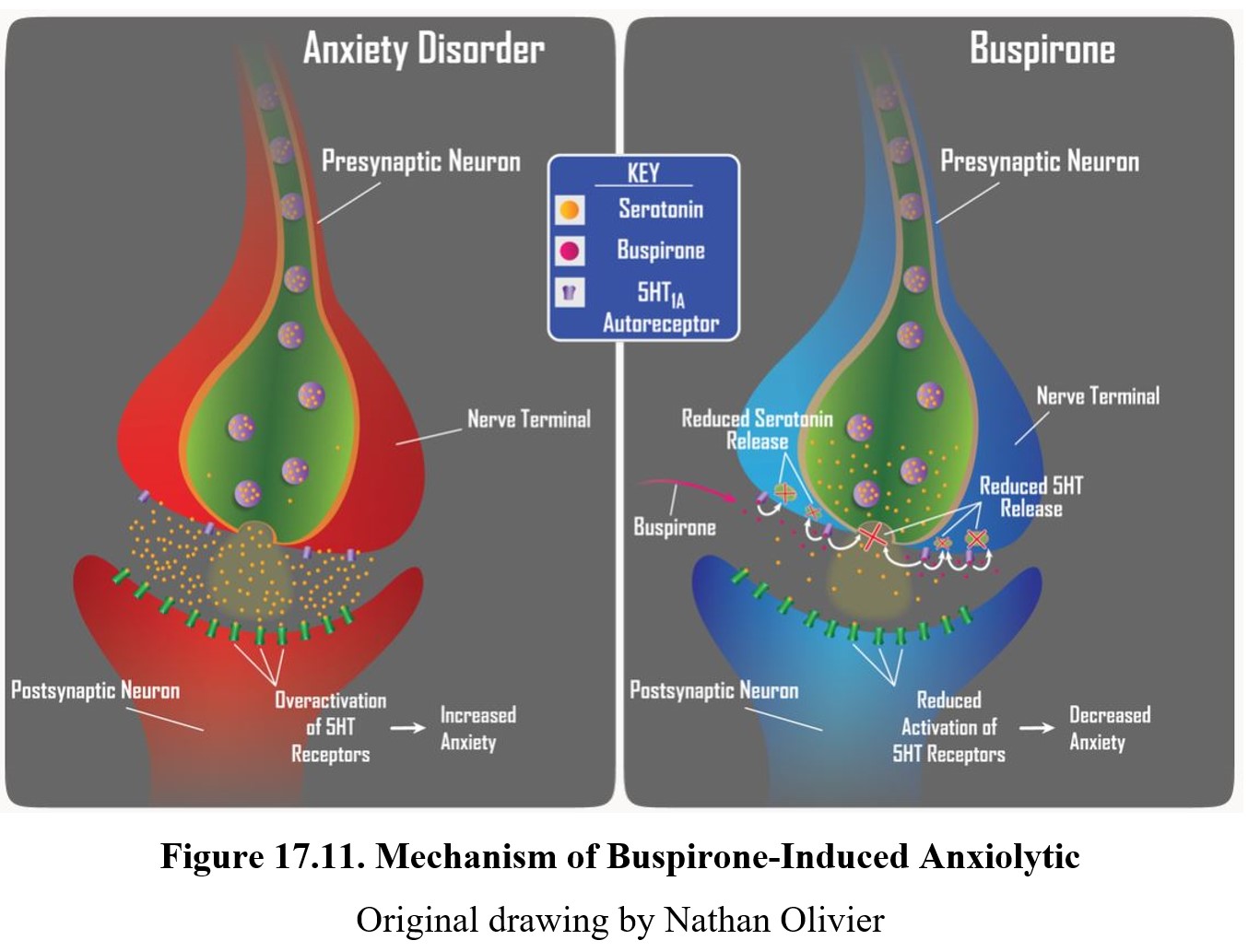
Because buspirone does not bind to GABAA receptors or alter GABA transmission in any way, it is not a sedative and is largely devoid of serious adverse effects. Buspirone can be taken in combination with alcohol without fear of synergistic CNS depression. This makes buspirone ideal for the treatment of anxiety, especially generalized anxiety disorder. Some side effects are still possible, including dizziness, nausea, and headache. Buspirone is sold under the trade name BuSpar®.
17.3.2. SSRIs Revisited
The use of SSRIs as antidepressants was covered in the previous chapter. They also have an application in treating anxiety. If you’ve been following along properly, this should seem confusing to you. According to the monoamine hypothesis of depression, SSRIs are effective because they raise serotonin levels in the limbic system. But the serotonin hypothesis of anxiety covered earlier in this chapter states that high levels of serotonin are the cause for anxiety. What’s going on here?
One hypothesis for how SSRIs might treat both depression and anxiety is that SSRIs only affect certain aspects of serotonin transmission. Consult the image below. The idea is that SSRIs work on synapses where the serotonin is activating 5-HT heteroreceptors on other serotonergic neurons. These heteroreceptors inhibit serotonin release at synapses related to anxiety. In other words, an “upstream” increase in serotonin levels causes a “downstream” decrease in areas related to anxiety.
Serotonin/norepinephrine reuptake inhibitors (SNRIs) are another type of antidepressant drug that shares the antianxiety effect of SSRIs.
How SSRIs and SNRIs Work for Anxiety [5:31]
Why SSRIs affect serotonin transport in some areas but not others is not fully understood. Indeed, the above explanation is only a prediction of how SSRIs might work. It is possible that SSRI effects on anxiety are mediated through different mechanisms, or that there are other factors involved besides serotonin activity. In short, we do not understand the effects with our current knowledge. Despite this, the effects are undoubtedly real. SSRIs are effective in treating various anxiety disorders.
17.3.3. Comparison of Anxiolytic Drugs
How do the anxiolytic drugs described above compare? Below is a table showing the preferred drug treatments for different anxiety disorders:
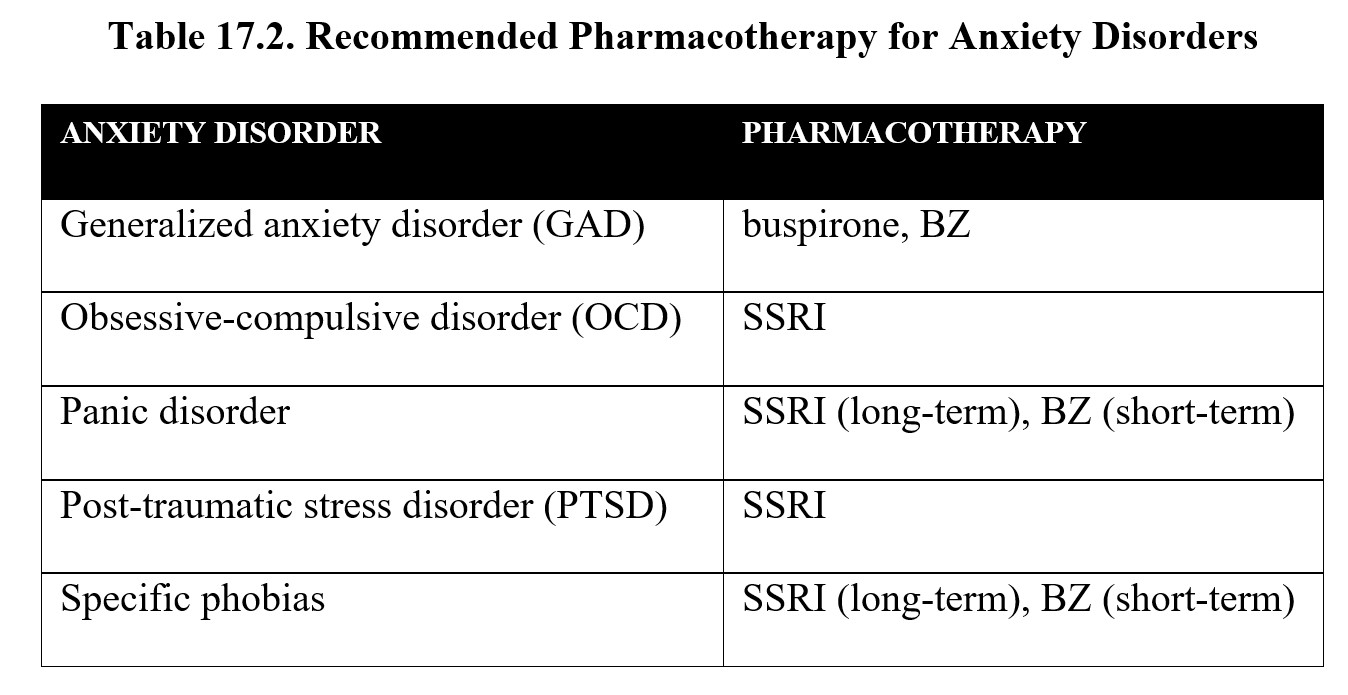
As you can see, SSRIs are preferred in the vast majority of cases. Their efficacy is comparable to benzodiazepines with fewer adverse effects. But their chronic use does not result in the development of dependence. Although SSRIs do run the risk of antidepressant discontinuation syndrome (see Chapter 16), this is mild when compared to the withdrawal effects seen in benzodiazepines. Still, the latter are sometimes used for short-term treatment. Benzodiazepines also remain relevant as drugs that can treat the withdrawal symptoms of other CNS depressants such as alcohol or barbiturates.
Before bringing this chapter to a close, we will briefly highlight one of the most recent advances in anxiety treatments. MDMA, which we covered in the chapter on psychedelics, was originally used to enhance psychotherapy, and this application has seen a comeback in recent years with research into MDMA-assisted psychotherapy. This may be an effective treatment for individuals with PTSD who are resistant to treatment, since MDMA may allow patients to be more willing to recall their traumatic memories during therapy. MDMA has potential application in drug-assisted psychotherapy.
Chapter Summary and Review
In this chapter, we took a close look at anxiety disorders and anxiolytic drugs. We identified not only the different types of anxiety disorders that can occur but also the brain structures and neurotransmitters involved in anxiety. We explored the history and uses of benzodiazepines, a major class of anxiolytic and sedative-hypnotic drugs, learning about their pharmacological profile and their action on GABAA receptors. We then examined two other drugs with anxiolytic effects, buspirone and SSRIs, and the alternate avenues through which they reduce anxiety. We ended the chapter by comparing these drugs and looking at the shifting landscape for anxiety medications.
Chapter 17 Practice Questions
Answer the following questions:
- What is the most common type of anxiety disorder?
- Abel sometimes gets panic attacks when he finds himself in crowded places. He finds the idea of being on a bus or plane terrifying and has started to stay inside his apartment for long periods. What anxiety disorder does Abel likely have?
- Which structure of the brain is responsible for conditioning fear responses?
- What role does the hypothalamus play in anxiety?
- What are two reasons why benzodiazepines replaced barbiturates?
- What are nonbenzodiazepines sometimes called? How do they differ from benzodiazepines?
- Explain why some benzodiazepines are long-acting.
- Do benzodiazepines directly activate GABAA receptors? Explain.
- What are the three main effects of benzodiazepines? What neurotransmitters are associated with these effects?
- There are two types of BZ receptors. Name them and describe which effects are controlled by each one.
- What does benzodiazepine withdrawal resemble?
- What receptor does buspirone interact with?
- Describe how SSRIs might influence serotonin transmission to reduce anxiety.
- Which type of drugs are most commonly used to treat anxiety disorders?
2nd edition