Chapter 19: ADHD and Alzheimer’s Drugs
2nd edition as of August 2022
Chapter Overview
For the fourth and final chapter on psychotherapeutic drugs, we will be examining medications used to treat ADHD and Alzheimer’s disease. Although these conditions have very little in common, they both involve chemical imbalances in the brain with behavioral consequences, yet neither is considered a mental disorder. ADHD is more properly classified as a neurodevelopmental disorder, while Alzheimer’s disease is a neurodegenerative disorder. In this chapter, we will explain what causes ADHD and Alzheimer’s and how certain drugs can be used to help treat them.
Chapter Outline
- 19.1.1. Symptoms and Prevalence
- 19.1.2. Causes of ADHD
- 19.1.3. Neurochemistry of ADHD
- 19.2.1. Amphetamine
- 19.2.2. Methylphenidate
- 19.2.3. Atomoxetine
- 19.2.4. Misuse of ADHD Medications
- 19.3.1. Types of Dementias
- 19.3.2. Symptoms and Prevalence
- 19.3.3. Causes of Alzheimer’s
- 19.3.4. Neurochemistry of Alzheimer’s
- 19.4.1. Cholinesterase Inhibitors
- 19.4.2. Memantine
- 19.4.3. Aducanumab
Chapter Learning Outcomes
- Describe ADHD to include its symptoms, prevalence, causes, and neurochemistry.
- Outline drugs used to treat ADHD and discuss issues with misuse.
- Describe Alzheimer’s disease to include its symptoms, prevalence, causes, and neurochemistry.
- Outline drugs used to treat Alzheimer’s disease.
19.1. ADHD
Section Learning Objectives
- Describe attention deficit hyperactivity disorder (ADHD) and its prevalence.
- Describe the three types of ADHD recognized by the DSM-5-TR and their diagnostic criteria.
- Explain the neurochemical basis of ADHD.
Chances are, you have heard of ADHD, or attention deficit hyperactivity disorder, or recognize it by its outdated name, attention deficit disorder (ADD). You may even know of someone who has been diagnosed with ADHD or have been diagnosed with it yourself. In this section, we will define ADHD and explore some of its potential causes.
19.1.1. Symptoms and Prevalence
Let’s begin this section by defining ADHD and its symptoms. Similar to previous chapters, this video by Osmosis is a good primer on most of the information we are about to cover, so give it a viewing before proceeding:
Attention Deficit Hyperactivity Disorder (ADHD/ADD) — causes, symptoms & pathology [6:08]
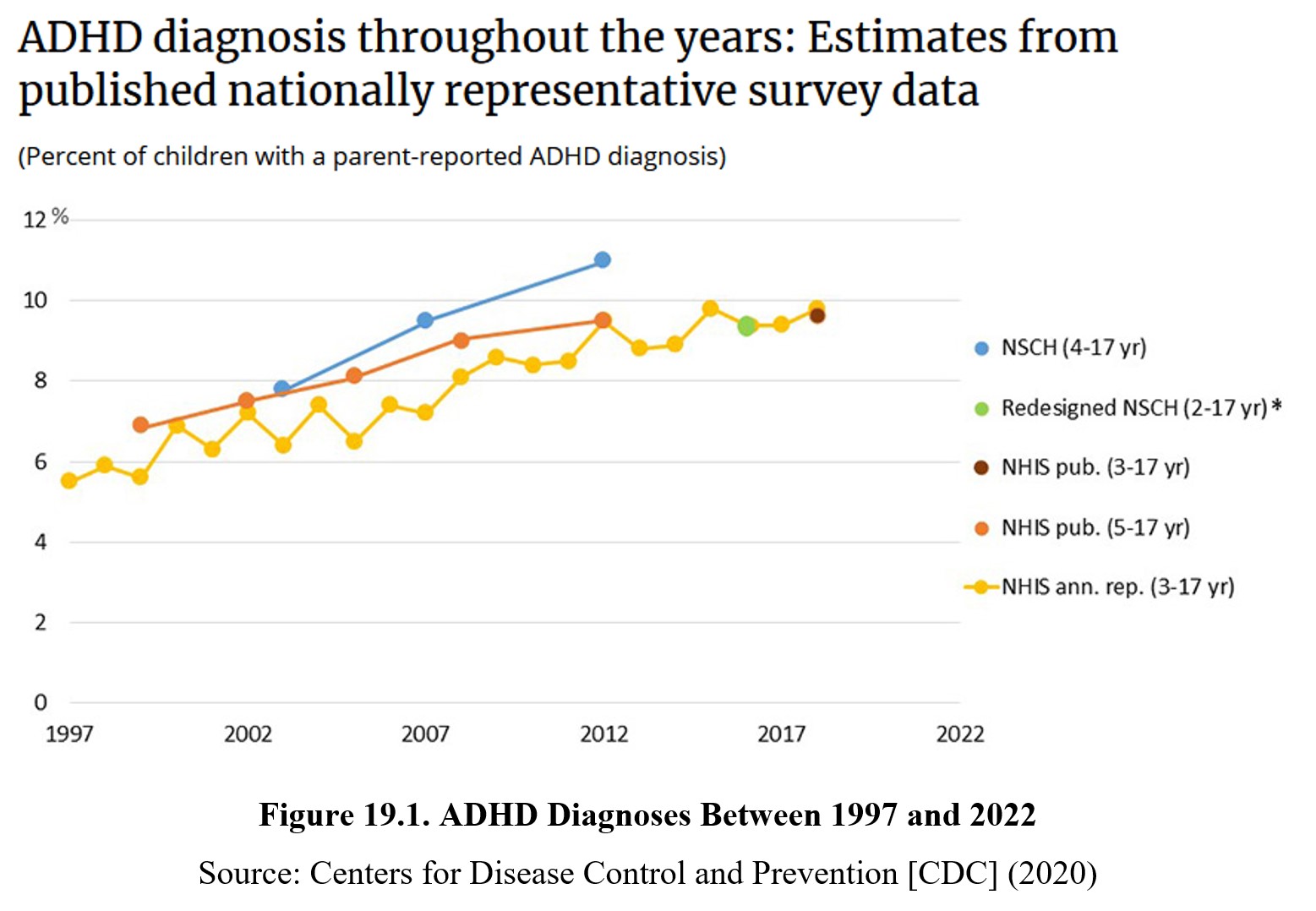
ADHD is a neurodevelopmental disorder that is characterized by inattentiveness and/or hyperactivity and impulsivity, as suggested by its name. It typically occurs in childhood but can persist into adulthood. About 9–10% of children and 5% of adults are diagnosed with ADHD. Boys are about three to four times as likely to be diagnosed. ADHD diagnoses are becoming increasingly common (see below), although the reason for the ten-year increase in prevalence of ADHD is unclear.
The DSM-5-TR currently recognizes three subtypes of ADHD: predominantly inattentive type, predominantly hyperactive-impulsive type, and combined type. Predominant inattentive type ADHD is mainly characterized by inattentiveness, while predominant hyperactive-impulsive type ADHD involves greater hyperactivity. As you might expect, combined type ADHD has both types of symptoms. Below is a list of symptoms associated with the two different types of ADHD:
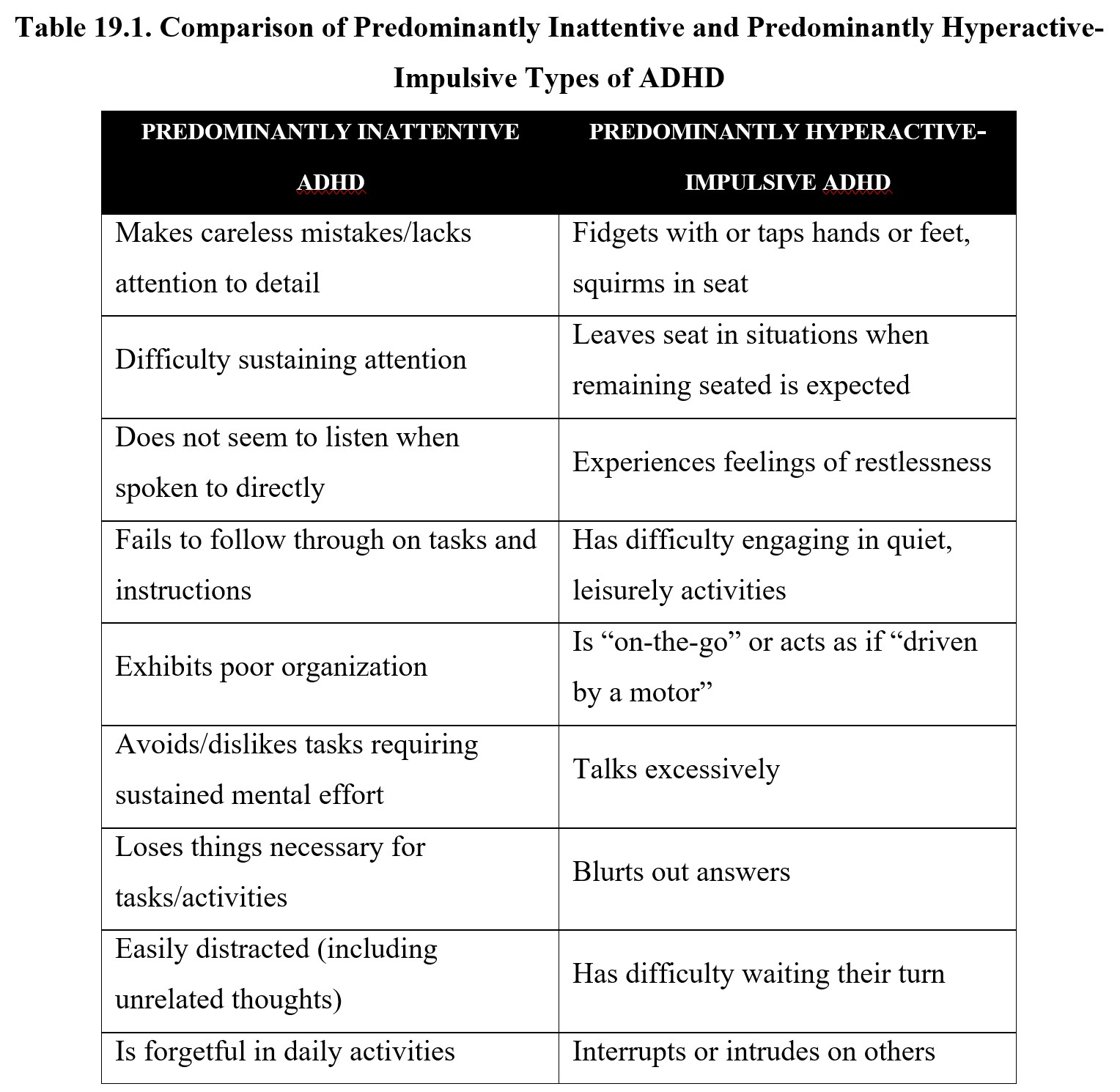
To be diagnosed with one of the two types under the DSM-5-TR, the individual must show at least five of nine possible symptoms for that subtype for at least six months. These symptoms should also be outside of normal development and interfere with social or academic/ occupational activities. If the criteria for both types are met, then the individual can be diagnosed with the combined type of ADHD.
19.1.2. Causes of ADHD
As mentioned in the video at the start of this section, the exact causes of ADHD are currently unknown. Genetics are involved since people with relatives who have been diagnosed with ADHD have an increased risk of developing the disorder themselves. The connection is likely complex, though, and may involve multiple genes and epigenetic interactions.
Because genetics cannot fully account for the development of ADHD, environmental factors are expected to play a role. There is much misinformation and a lot of false beliefs about what might contribute to ADHD in children. Some causes, such as eating sugary foods, watching too much television, sucking on baby furniture with lead-based paints, certain parenting styles, and social factors have all been suggested at one time or another to be related to the development of ADHD.
Factors that interfere with early neurodevelopment, such as drug use during pregnancy, premature birth, exposure to toxins, or brain injuries, have been linked with an increased risk (NIMH, 2016). Recent studies have also linked prenatal exposure to acetaminophen to a higher risk of ADHD (Ystrom et al., 2017).
Part of the difficulty in determining the causes of ADHD lies in the fact that many other problems can occur in childhood that can give rise to ADHD-like symptoms. For instance, children with hearing or vision problems may exhibit some of the behavioral tendencies of children with ADHD because they are unable to focus on a teacher’s voice or presentation.
19.1.3. Neurochemistry of ADHD
As in the case of the disorders discussed in previous chapters, ADHD is thought to be caused in part by a chemical imbalance in the brain. The two neurotransmitters implicated in ADHD are norepinephrine and dopamine. It is thought that low levels of norepinephrine and dopamine activity in the limbic system and prefrontal cortex cause the inattentiveness, impulsivity, and hyperactivity seen in ADHD. Examine the diagram below:
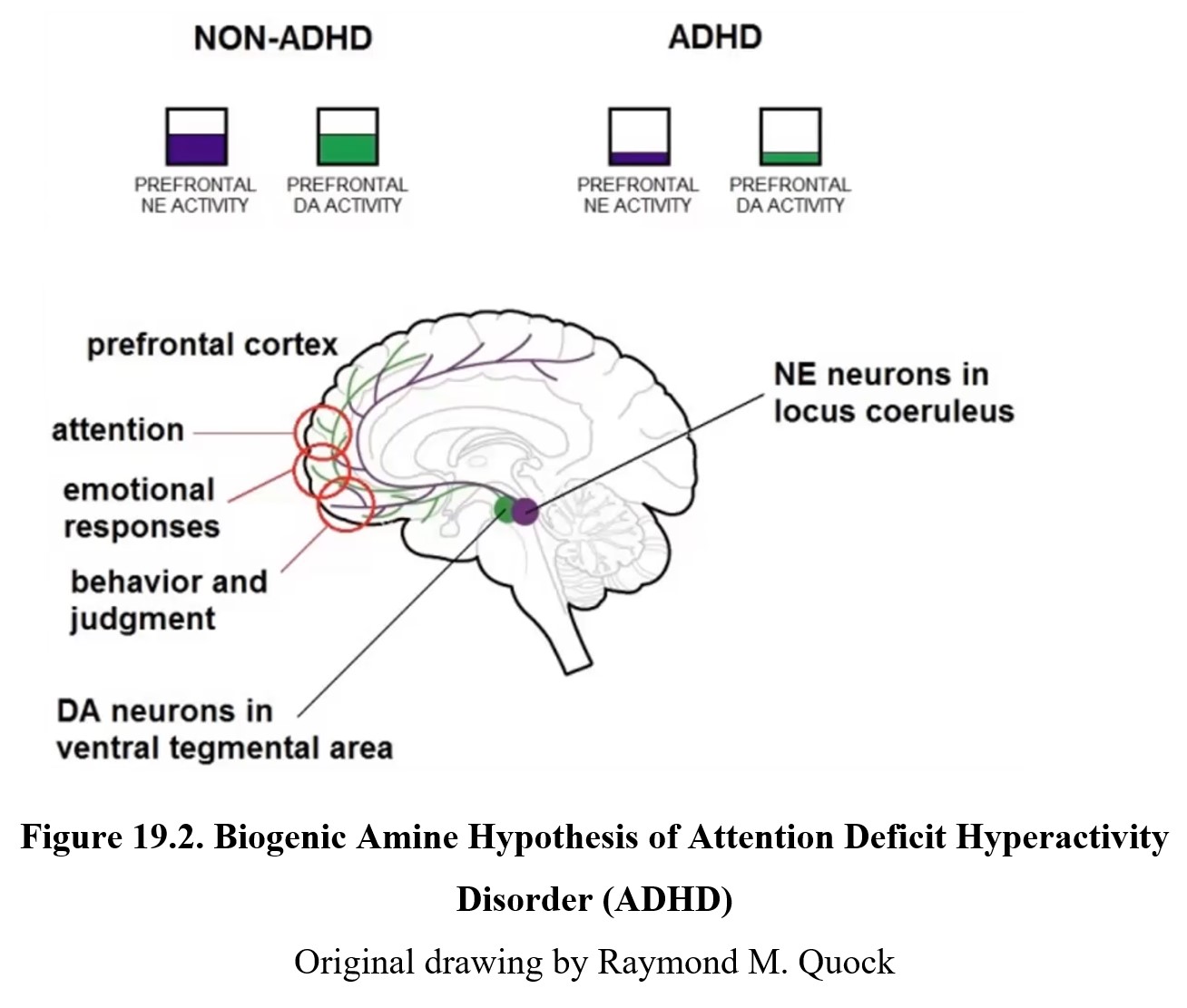
By now you should be familiar with how dopamine neurons in the ventral tegmental area (VTA) project to the limbic system and prefrontal cortex. This is part of the reward system, which regulates motivation and involves areas that are responsible for our emotional responses and judgments. It is thought that low levels of dopamine activity in the limbic system contribute to the symptoms seen in predominantly hyperactive-impulsive type ADHD since these low levels mean our brain is constantly seeking stimulation and experiencing stronger impulses than normal.
Norepinephrine neurons in the locus coeruleus (Latin for “blue spot”) project along similar pathways as the dopamine neurons discussed above. These neurons reach areas in the prefrontal and frontal cortex that are responsible for executive functions, cognitive processes that include attention, working memory, and the ability to tune out distractions or suppress impulses. As you might suspect, disruption of these executive functions due to low norepinephrine activity is associated with inattentive type ADHD. Compare the two in the diagram below.
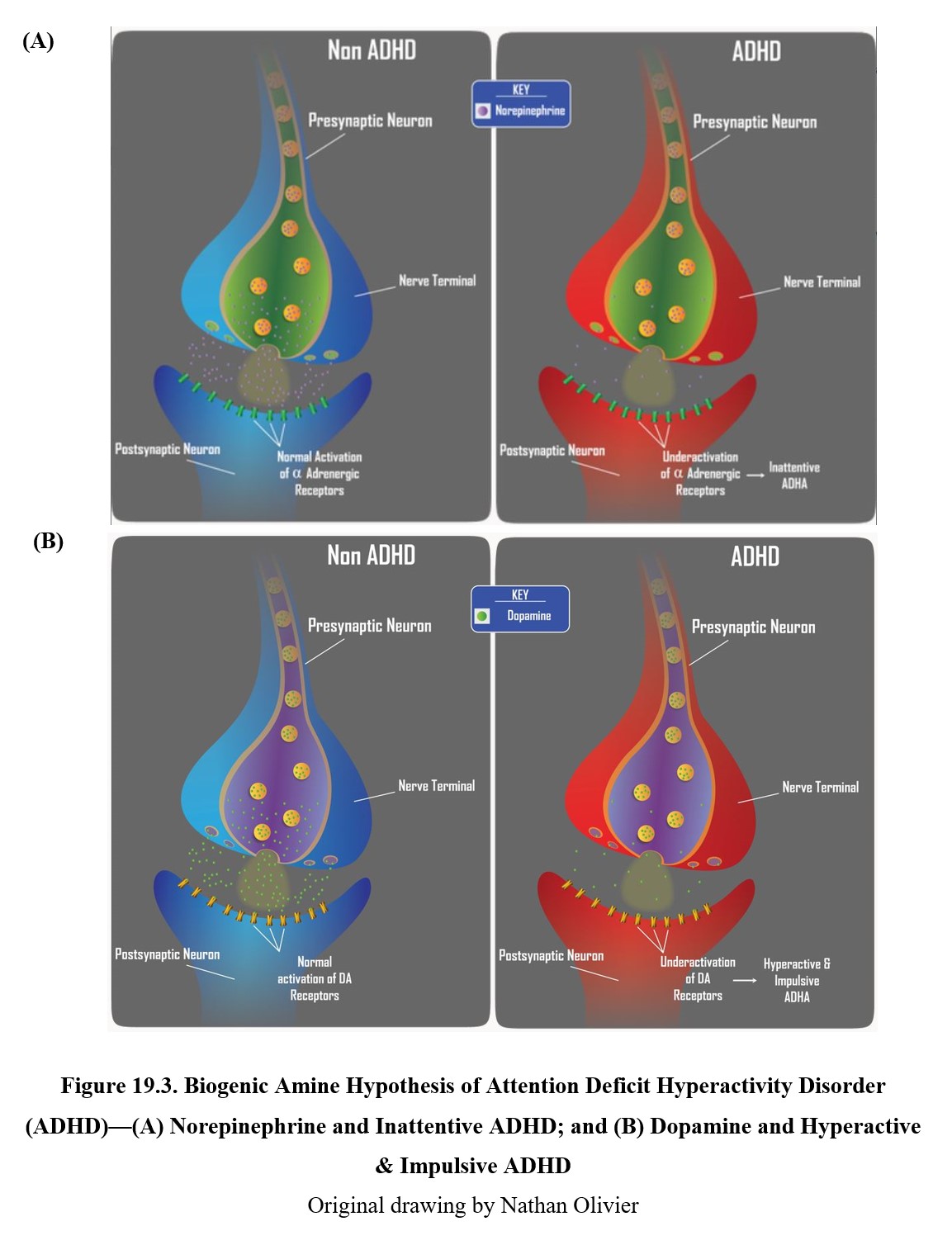
The role of norepinephrine (panels on the left) and dopamine (panels on the right) in ADHD. In non-ADHD cases, a regular amount of norepinephrine and dopamine is released, leading to normal activation of adrenergic and dopaminergic receptors (upper panels). Low levels of norepinephrine activity are associated with inattentive type ADHD (lower left panel), while low levels of dopamine activity are associated with hyperactive-impulsive type ADHD (lower right panel).
19.2. ADHD Drugs
Section Learning Objectives
- Explain the mechanisms of action and effects of drugs used to treat ADHD.
- Discuss the adverse effects and misuse of ADHD medications.
Now that we understand the neurochemical basis for ADHD symptoms, we can discuss the different types of drugs used to treat ADHD. Although there are some exceptions, the most common medications are CNS stimulants such as amphetamine.
Stimulants for Hyperactivity?
At first glance, giving stimulants to children who already have problems sitting still and focusing seems like it would only make the problem worse. However, remember that stimulants increase levels of norepinephrine and dopamine, which is why they can have a therapeutic effect on ADHD symptoms, which are caused by low levels of these transmitters.
If you are still confused by the idea, consider watching the video below by Hank Green of SciShow:
Why Stimulants Help ADHD [6:08]
It should be noted that aside from medications, ADHD can also be addressed with certain behavioral therapies. Our discussion in this section, however, will be limited to the drugs used in pharmacotherapy.
19.2.1. Stimulants
The classic treatment of ADHD involves stimulants. You may remember the discussion of Adderall®, a non-racemic amphetamine mixture, from the chapter on high-efficacy stimulants. You might also recall that another possible clinical use for methamphetamine is the treatment of ADHD. It is sold under the brand name Desoxyn® and is considered a second-line treatment for ADHD (amphetamine and methylphenidate are the first-line medications). These medical uses keep amphetamine and methamphetamine Schedule II drugs, rather than Schedule I.
The actions of Adderall® and Methedrine® are the same as what was covered in that chapter, so we will only quickly go over the main points again. Amphetamine and methamphetamine reverse the transport proteins responsible for reuptake of monoamines, causing them to pump out more neurotransmitter into the synapse. This increases the activation of norepinephrine and dopamine receptors, reducing ADHD symptoms (see below).
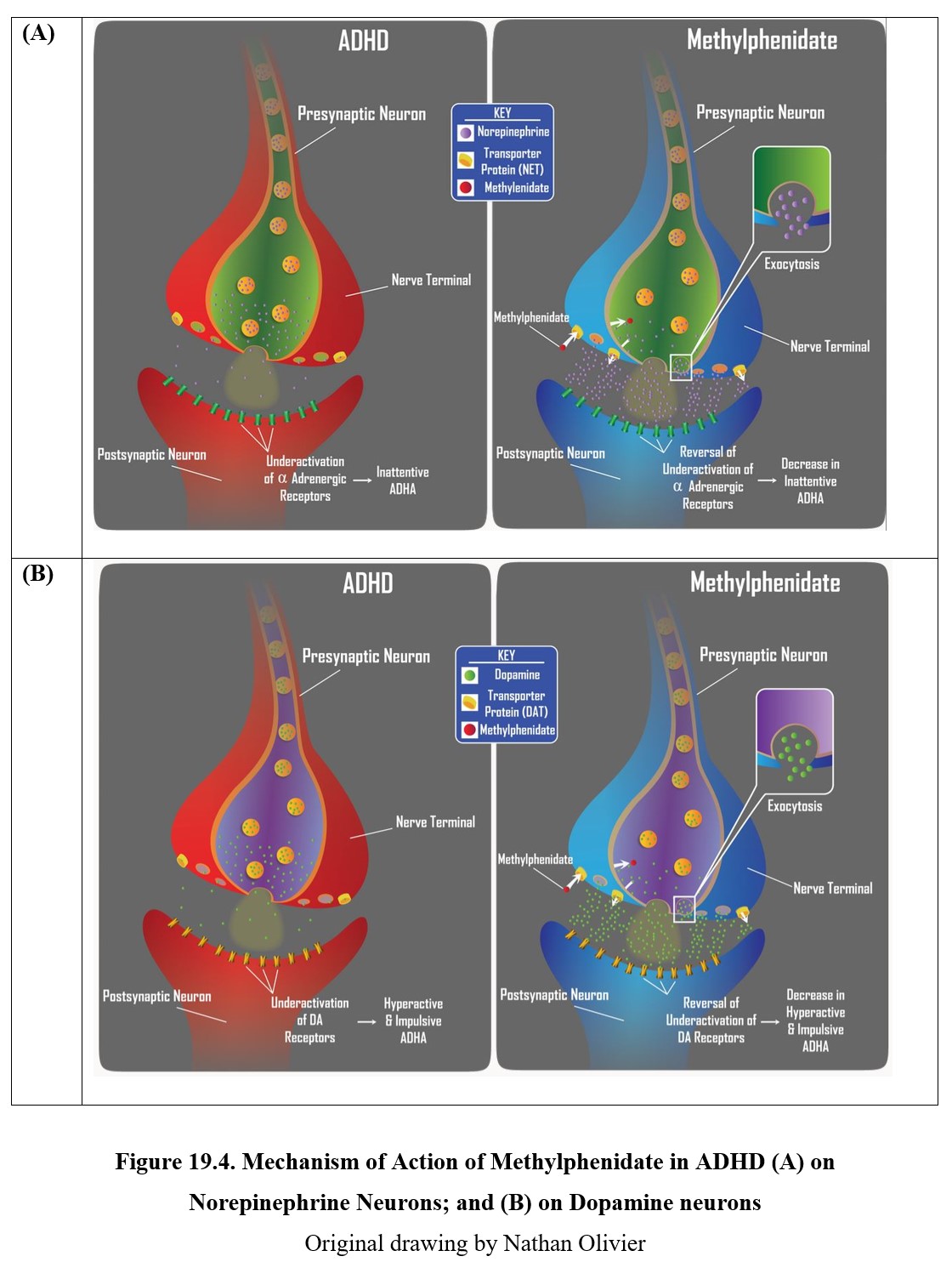
Another stimulant that is used to treat ADHD is methylphenidate, which you may recognize by its brand names Ritalin® or Concerta®. It is classified as a norepinephrine–dopamine reuptake inhibitor (NDRI). Instead of reversing the transport proteins like amphetamine, methylphenidate simply blocks the reuptake of norepinephrine and dopamine.
Although stimulants are typically considered drugs of abuse, the stimulants prescribed for treatment of ADHD are relatively safe. When used appropriately (i.e., in correct doses by someone with ADHD), they do not cause euphoria and can be used for long periods without development of tolerance or physical dependence. This is because medications such as Adderall® cause a slow, extended release of neurotransmitter that is sufficient for therapeutic effects without causing euphoria or dependency. If taken in larger doses, however, they can produce euphoria and be misused for recreational purposes.
Misuse of amphetamine or methylphenidate can lead to high blood pressure, irregular heart rate, sleep disturbances, and loss of appetite. Like other CNS stimulants, they can also cause seizures, bruxism (grinding of the teeth), and open sores in the skin. Psychological effects include anxiety, tension, disruption of memory, aggression, and psychosis. Again, it is important to note that these effects are not seen during therapeutic use.
19.2.2. Atomoxetine
An alternative to stimulants, atomoxetine (Straterra®) was originally developed as an antidepressant before becoming an ADHD treatment. It is a selective norepinephrine reuptake inhibitor (NRI), which means it blocks reuptake of norepinephrine (see figure below). This causes atomoxetine to have a greater effect on reducing symptoms of inattentive type ADHD. Parents generally prefer atomoxetine to other anti-ADHD medications for the simple reason that atomoxetine does not cause stimulation.
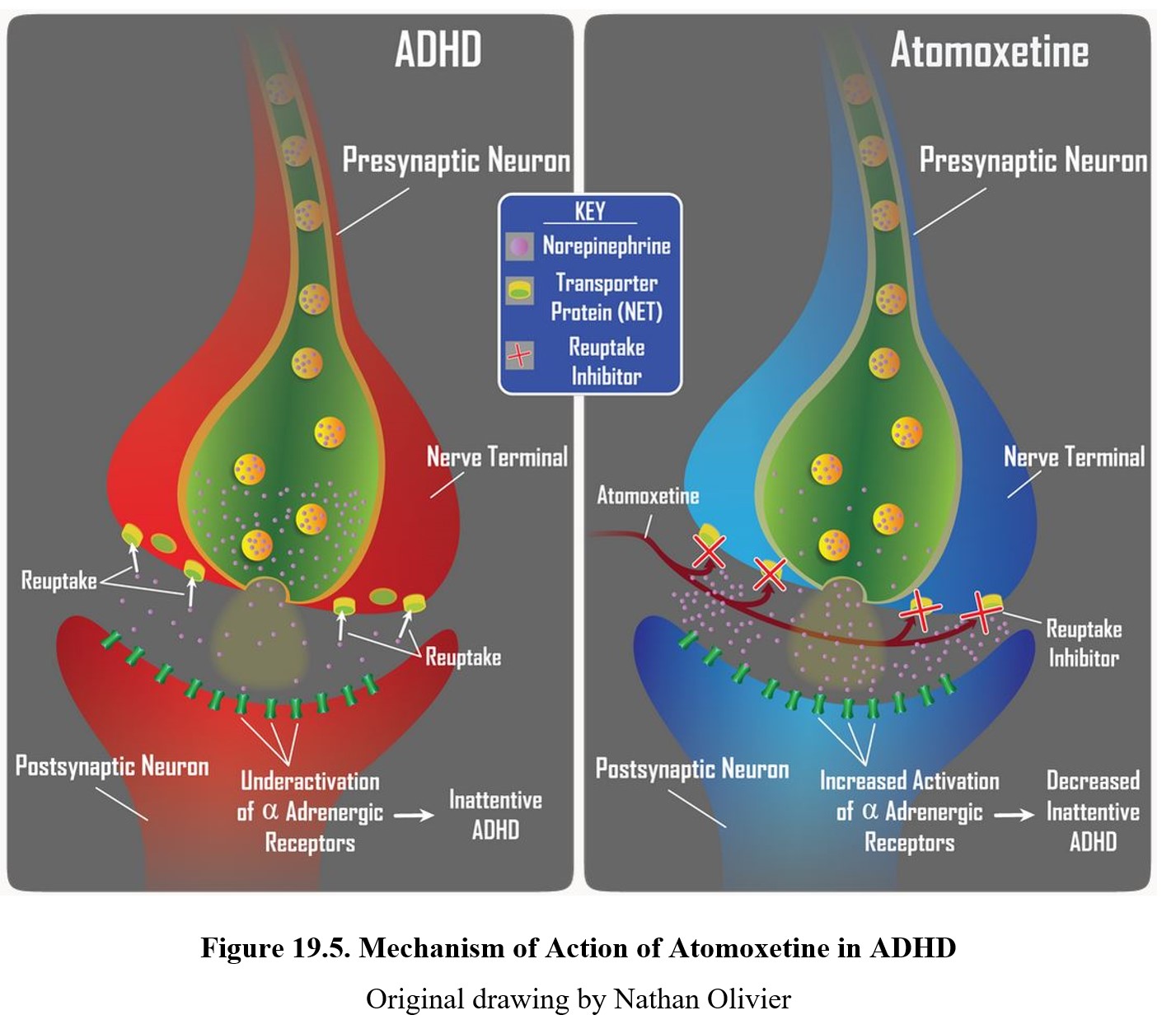
Side effects of atomoxetine include reduced appetite, dry mouth, mood swings, and tiredness. Unlike amphetamine, atomoxetine has no potential for abuse. At the same time, it is less effective than traditional stimulants, with significant residual symptoms seen in 40% of ADHD patients. Because of this, it is viewed today as a second-line treatment that may be combined with stimulants for treatment.
19.2.3. Misuse of ADHD Medications
As mentioned previously in both this section and Chapter 8, stimulants prescribed for treatment of ADHD are often misused by people who do not have ADHD for a variety of purposes. Because they suppress appetite, some people use amphetamine for weight loss; others simply enjoy the euphoria and use it to get high. One of the most common uses involves taking amphetamines (such as Adderall®) in order to boost performance in physical or cognitive activities.
Although the expectation is that drugs like Adderall® or Ritalin® will help you focus and improve your memory when studying. In reality, there is little evidence that they enhance cognition in people without ADHD. Studies have indicated that stimulants do provide a modest improvement to certain cognitive processes in healthy adults, but these changes only occur at low doses and may actually reflect improvements in energy and motivation combined with the placebo effect.
ADHD medications, especially Adderall®, have garnered an undeserved reputation as a cognitive enhancer. As such, they are misused by college students who believe that they will become smarter as a result of taking the pills prior to an examination. The answer is quite complicated. It is a fallacy to believe that all drugs will work all the time. This is simply not the case. In this unit, we have examined the mood-elevating effects of antidepressant drugs. But these drugs will elevate the mood only if the person taking the drug is mentally depressed. If the drug user is not depressed, antidepressants will not increase the person’s mood.
Some drugs but obviously not all drugs work only when a system is malfunctioning. In the person with ADHD, there is a chemical imbalance that disrupts attention and self-control. Adderall® can correct the chemical imbalance and, indeed, enhance cognition. But in an individual who does not suffer from ADHD, Adderall® has no effect on those cognitive functions because they are intact. Persons without ADHD will swear that the drug is a cognitive enhancer and perform marvelous on the exam the next day. But there is a property of amphetamine that is always there; it is the stimulant action of amphetamine. Not being able to sleep, the person stays up and studies, which explains the high exam score. But that is the result of the stimulant property of amphetamine and not because amphetamine made you smarter. Studies have shown that ADHD medications do not enhance cognition or academic performance in users who do not suffer from ADHD (Arria et al., 2017).
19.3. Alzheimer’s Disease
Section Learning Objectives
- Define dementia and provide several examples of causes of dementia.
- Define the most common characteristics of Alzheimer’s disease.
- Describe the pathology of Alzheimer’s disease, including amyloid plaques and neurofibrillary tangles.
- Explain the acetylcholine and glutamate hypotheses of Alzheimer’s disease.
Alzheimer’s disease, also referred to simply as Alzheimer’s, is a disease of the brain characterized by memory loss and the gradual deterioration of other cognitive functions. Alzheimer’s is progressive, meaning it worsens over time. Before discussing Alzheimer’s medications, we will first explore the symptoms and causes of Alzheimer’s disease.
19.3.1. Types of Dementias
Alzheimer’s disease is a type of dementia, which is a group of common symptoms that include declines in memory, language and thinking skills, and ability to perform everyday activities. Dementia is distinct from normal aging or regular cognitive lapses and involves an abnormal, progressive and disabling decline in cognitive functions. There is no cure for dementia, although certain treatments can help slow the decline or reduce symptoms.
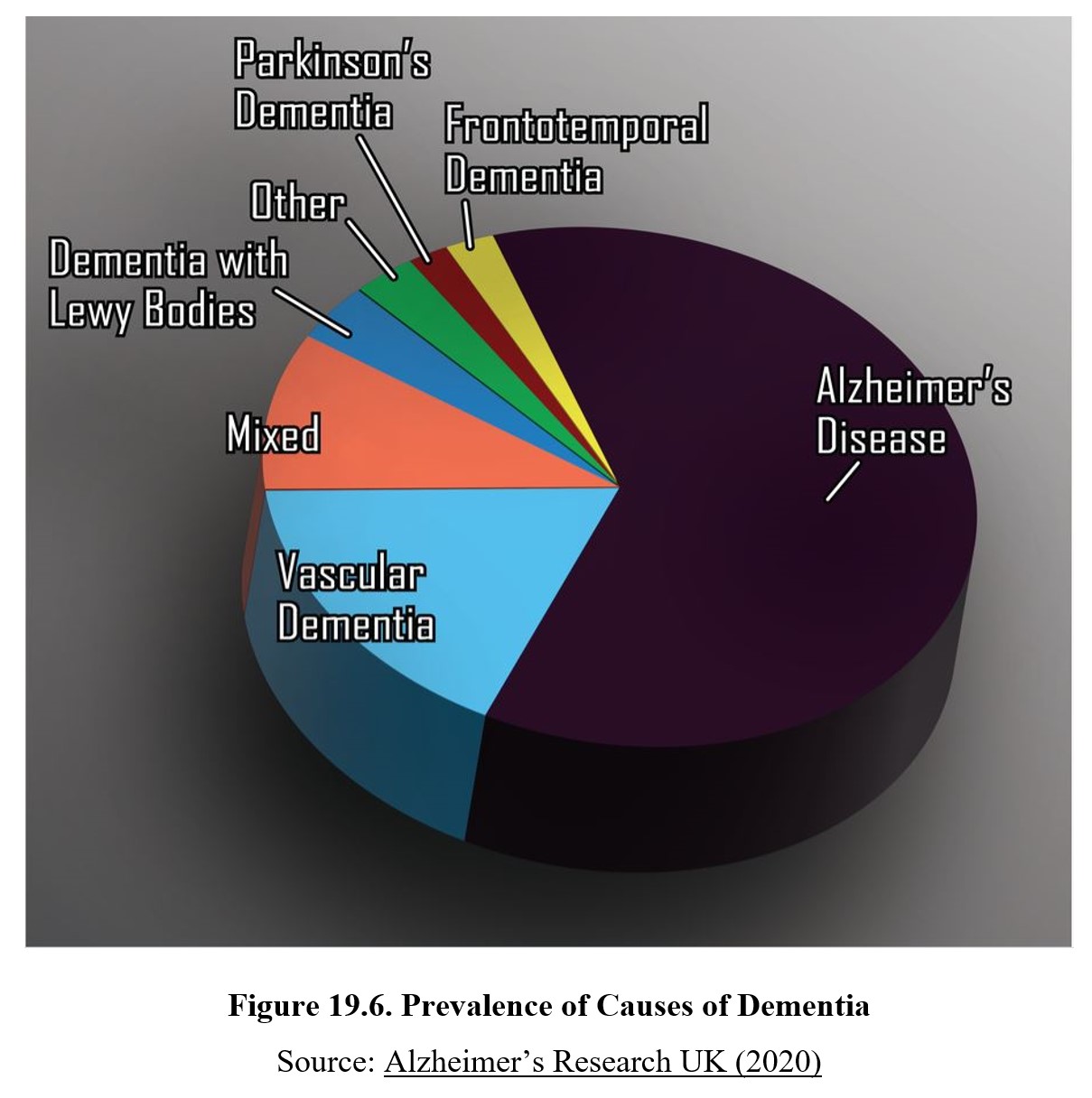
Dementia is not a disease itself and can be caused by a variety of disorders. Alzheimer’s is the most common cause of dementia by far, responsible for 60–70% of cases. We have also mentioned Parkinson’s disease and Huntington’s disease before. Both can lead to dementia. Korsakoff syndrome caused by excessive alcohol use is another example. The greatest risk factors for Alzheimer’s disease are genetics and aging.
Aside from Alzheimer’s disease, the next most common cause of dementia is vascular dementia. The term vascular refers to blood vessels, so vascular dementia is caused by an issue with blood supply to the brain. This can be caused by blockages, reduced blood flow, or rupture of the blood vessels. People who have conditions that affect the vascular system, such as high blood pressure or cholesterol, diabetes, cardiac arrhythmias, or a history of smoking are at an increased risk for developing vascular dementia.
The symptoms of vascular dementia depend on where in the brain blood supply is disrupted. For instance, if the hippocampus is affected, the patient is likely to experience memory loss. People with vascular dementia often experience multiple minor strokes or stroke-like episodes that contribute to the cognitive decline seen in dementia.
The third-most common type is mixed dementia, which denotes dementia with multiple causes. This is relatively common because many types of diseases can cause or co-occur with other diseases. Progression of Alzheimer’s disease can often occur alongside the development of vascular dementia, for example.
There are many other possible causes of dementia, including dementia with Lewy bodies, frontotemporal dementia, HI6V-associated dementia, and others. We won’t cover all of them in detail. It is sufficient to be able to describe the three main types for this class and recognize that there are numerous examples. You can compare the rates of different causes in the chart below:
19.3.2. Symptoms and Prevalence
The principal signs and symptoms of Alzheimer’s disease are:
- Amnesia, loss of ability to recall one’s memories
- Apraxia, loss of ability to execute motor movements
- Aphasia, loss of ability to comprehend and express speech
- Agnosia, loss of ability to process sensory information, which can include visual, auditory, tactile, or olfactory senses
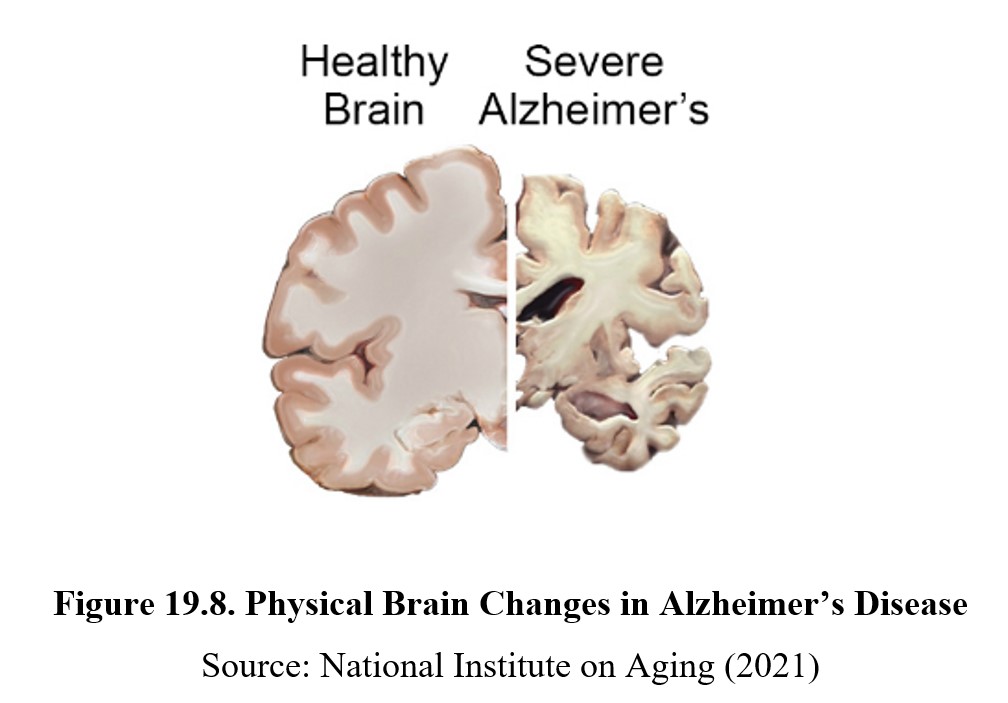
Alzheimer’s is a neurodegenerative disease, meaning that over time, neurons in the brain will degrade and die. This disrupts normal functioning and leads to the main symptoms of Alzheimer’s, such as loss of memory and language skills. Compare the composition of a normal brain to one with Alzheimer’s in the image below. Deterioration of both white and gray matter in the brain leads to a reduced volume and enlarged gaps. This deterioration occurs in the hippocampus first, which causes the decline in memory, followed by the areas in the temporal lobe responsible for language.
Alzheimer’s progresses in stages, from mild to moderate to severe. Mild or early-stage Alzheimer’s involves symptoms that may not be obvious but can be detected by close friends and family. Individuals may be unable to remember a word or name, show changes in their mood or personality, and may show diminished judgment. At this stage, people with Alzheimer’s are still capable of living their lives independently.
Once Alzheimer’s reaches the moderate or middle-stage, symptoms become more pronounced. People may be unable to remember events in their personal history or learn new information, and changes in behavior and personality may be significant and abrupt. They might also become agitated, aggressive, or confused and find themselves lost or wandering aimlessly. People with moderate Alzheimer’s require some assistance in their daily lives, although they may still be able to handle simple tasks.
Finally, severe or late-stage Alzheimer’s involves extreme disruptions in cognitive functions. During this stage, patients may lose control over movement or other physical abilities such as holding objects or swallowing. Communication may be difficult or impossible. By late-stage Alzheimer’s, afflicted individuals may be bedridden and require continual assistance and long-term care.
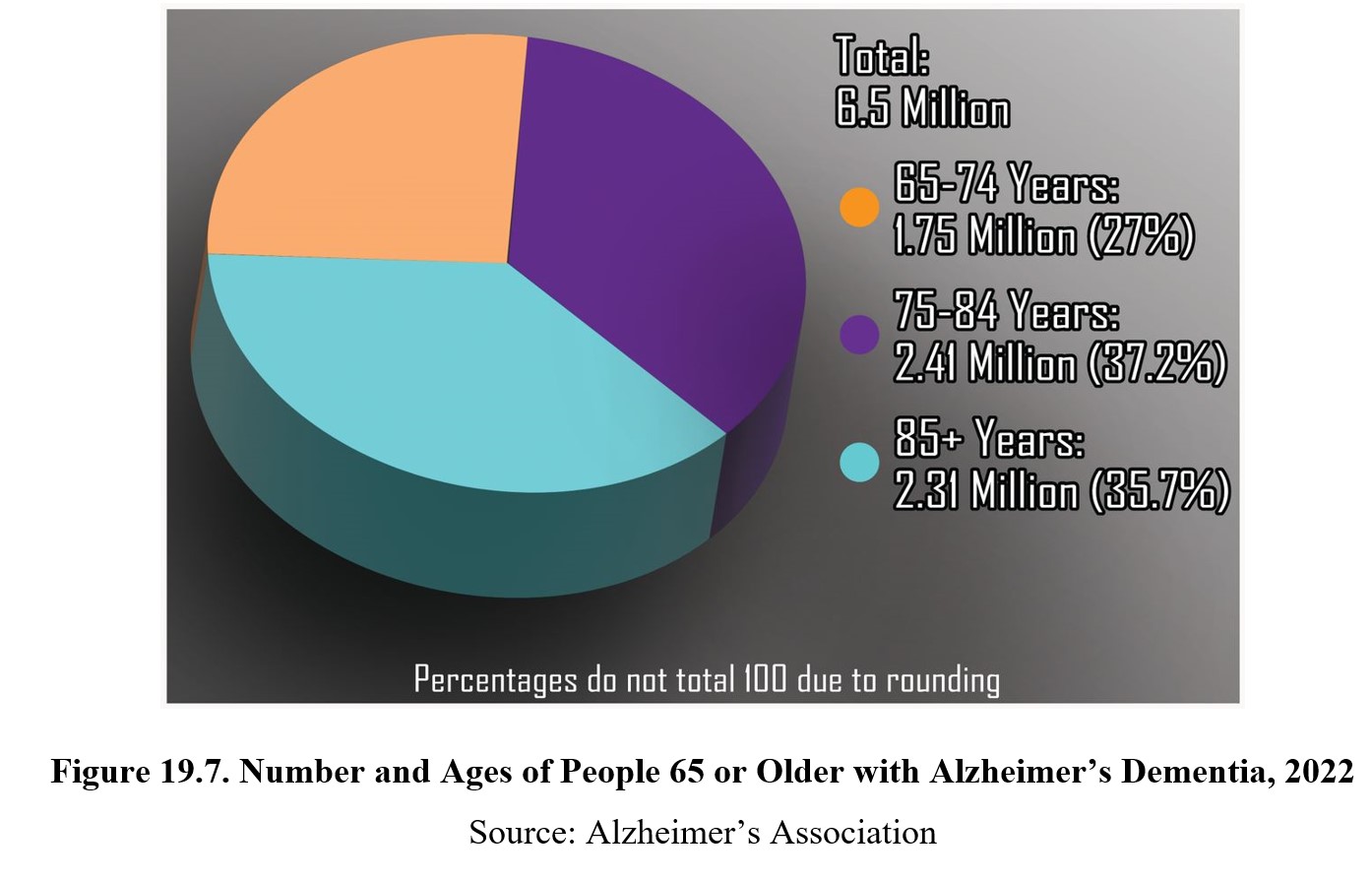
Alzheimer’s is a terminal illness and there is no way to stop or reverse its progression. The life expectancy is typically 3–9 years, depending on the time of diagnosis and severity of the disease. The onset of Alzheimer’s usually occurs older than 65, with increased rates at higher ages. About 6% of all people over the age over the age of 65 are diagnosed with Alzheimer’s. If Alzheimer’s is diagnosed before 65, it is considered early-onset Alzheimer’s. Only about 5–10% of all Alzheimer’s cases are early-onset.
19.3.3. Causes of Alzheimer’s
What causes the neurodegeneration seen in Alzheimer’s disease? There are two consistent features of Alzheimer’s disease that may explain how the degeneration occurs. These features are amyloid plaques and neurofibrillary tangles.
How Alzheimer’s Changes the Brain [3:59]
Amyloid plaques are hard, insoluble buildups that can be found outside of neurons in people with Alzheimer’s. They are comprised mainly of amyloid beta (Aβ), protein fragments that are cleaved off of amyloid precursor proteins. In healthy brains, Aβ is broken down further and eliminated. In Alzheimer’s, however, these fragments accumulate and form the amyloid plaques seen in the illustration above.
In comparison, neurofibrillary tangles occur inside the neuron. As the name suggests, these are tangles of neurofibrils called microtubules that help transport nutrients within the cell and maintain its structure. Microtubules found in the axons of neurons are stabilized by tau proteins. These proteins are abnormal in Alzheimer’s disease and cause the microtubules to break down, forming tangled clumps of insoluble fibers.
Both amyloid plaques and neurofibrillary tangles interfere with normal cell functioning and can cause neurons to deteriorate or die due to a lack of nutrients or other essential functions being impaired. The reason why plaques and tangles accumulate in people with Alzheimer’s but not in healthy individuals is not fully understood. Genetics and environmental factors are both believed to play a role. Numerous genes have been implicated as risk factors, while other behaviors such as smoking can increase risk.
19.3.4. Neurochemistry of Alzheimer’s
One of the older explanations for Alzheimer’s involved the neurotransmitter acetylcholine. This idea, called the Cholinergic Hypothesis, suggested that low levels of acetylcholine activity in the hippocampus was responsible for the memory loss seen in Alzheimer’s disease. Although we now know that this is not the direct cause, acetylcholine still plays an important role in memory formation and Alzheimer’s symptoms. Examine the figure below:
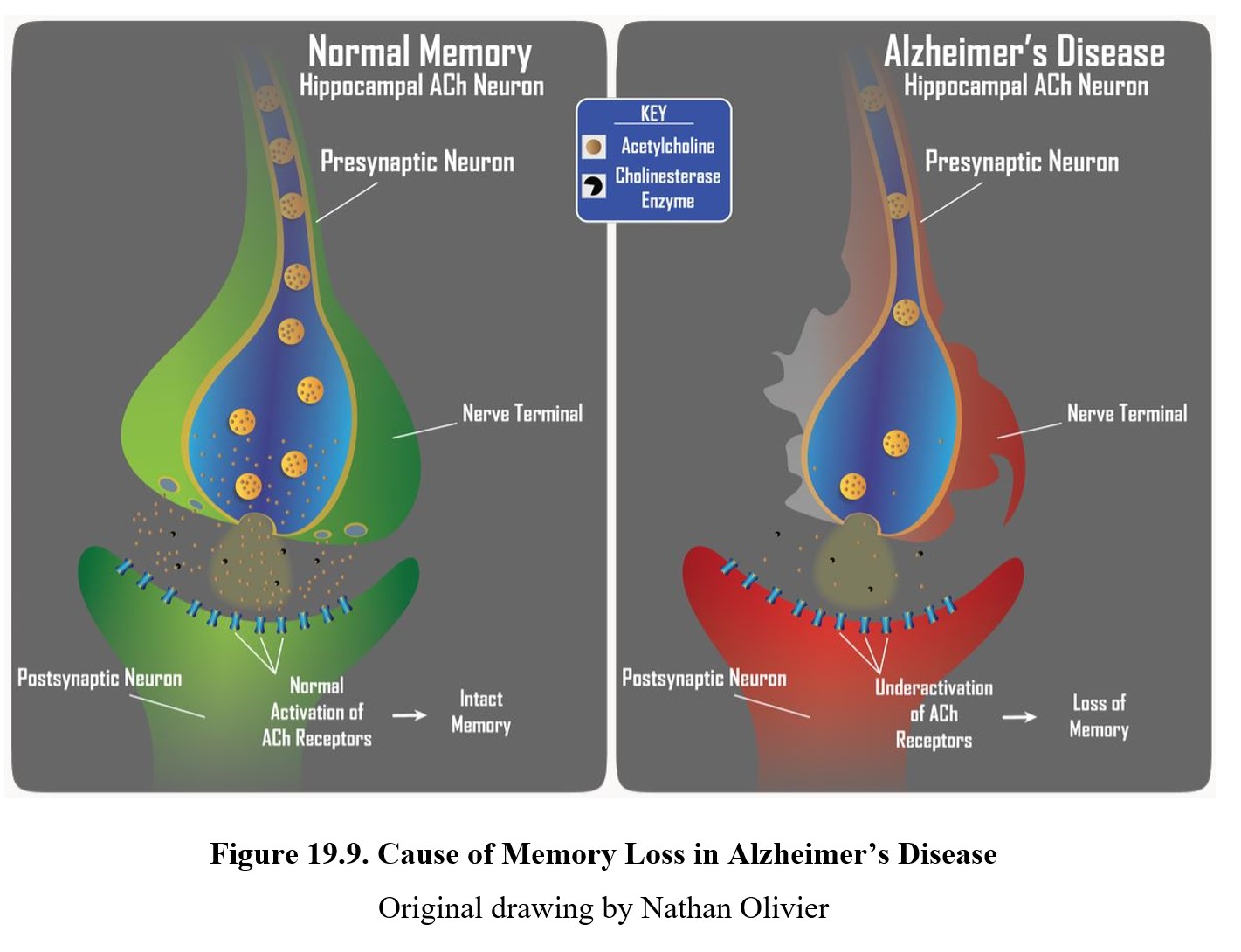
In the upper panel, you can see how normal activation of cholinergic receptors in the hippocampus is involved in memory. In Alzheimer’s disease, acetylcholine levels are reduced because of the deterioration of neurons (lower panel). This results in loss of memory and difficulty forming new memories in patients with Alzheimer’s.
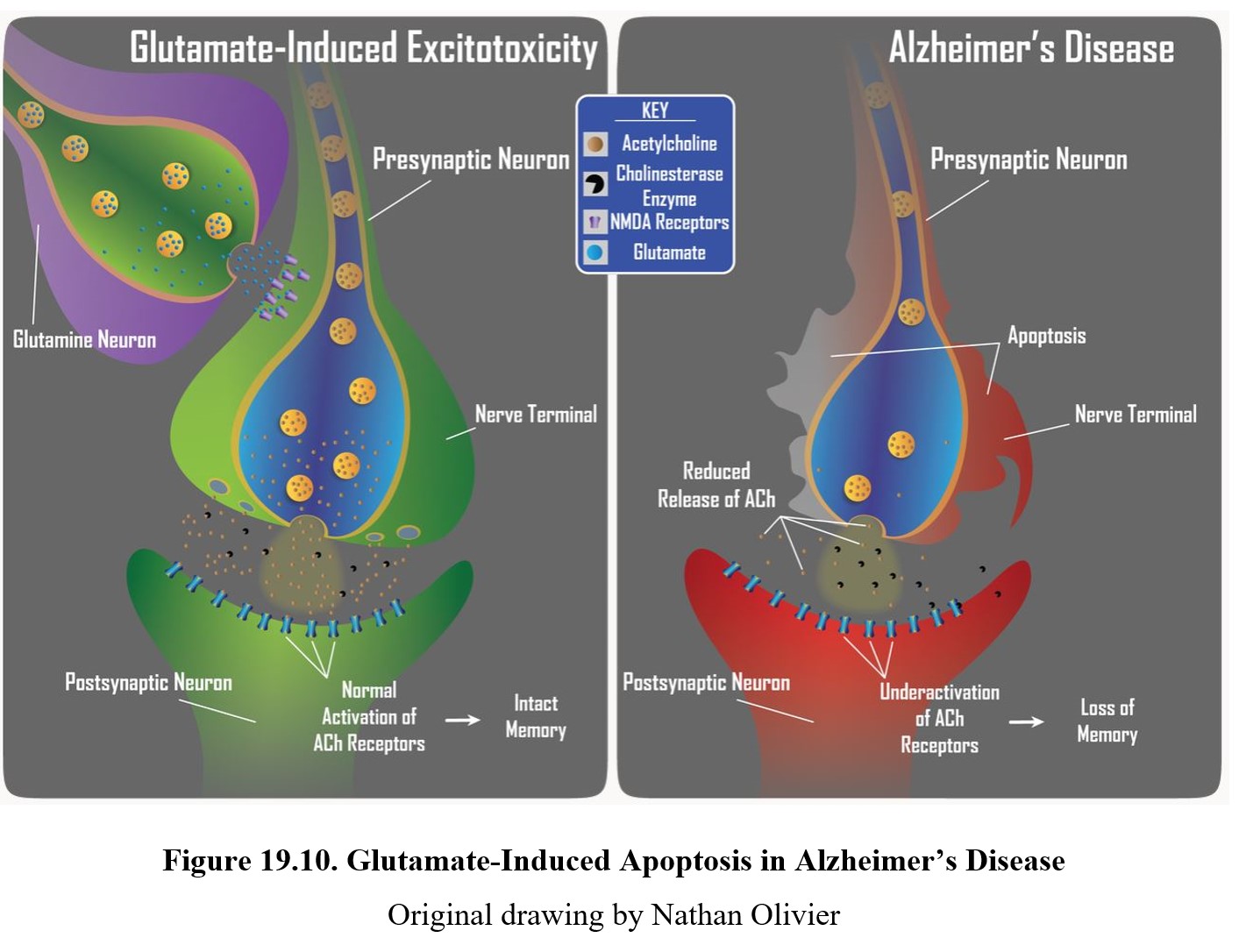
Another neurotransmitter that is involved in neurodegenerative diseases such as Alzheimer’s is glutamate. Glutamate is an excitatory transmitter that is involved in apoptosis, or programmed cell death. Apoptosis is a regular and necessary mechanism for disposing of cells that are no longer needed or have been compromised by infections.
Apoptosis is triggered by a large release of glutamate outside the target cell by other neurons or glial cells. The glutamate binds to and activates NMDA receptors, which are ionotropic receptors that allow calcium ions to enter the cell. In normal levels, this depolarizes the cell, but at extreme levels the calcium ions activate enzymes that damage cell structures and eventually result in cell death.
In Alzheimer’s disease, damaged or diseased neurons or glial cells can release excessive amounts of glutamate (upper panel). This results in excitotoxicity, whereupon neurons are unnecessarily damaged or killed. This figure below shows how excitotoxicity can turn a healthy neuron into a deteriorating one (lower panel). This reduces synaptic activity and leads to Alzheimer’s symptoms like memory loss or cognitive impairment.
19.4. Alzheimer Drugs
Section Learning Objectives
- Describe the use of psychotherapeutic agents to slow memory loss and cell death in Alzheimer’s disease.
As mentioned in the previous section, there is no cure for Alzheimer’s disease. The objective of Alzheimer treatment is to enhance the quality of life by enhancing functional performance and improving behavior, cognition, and mood. There are several treatments that can slow the progression of the disease or alleviate some of its symptoms. In this section we will look at the two types of drugs that have therapeutic effects on Alzheimer’s disease.
19.4.1. Cholinesterase Inhibitors
The first type of drugs we will discuss are cholinesterase inhibitors. Cholinesterase is an enzyme that breaks down acetylcholine into acetic acid and choline. Cholinesterase enzymes are responsible for removing acetylcholine from the synapse. In the figure below, they are represented by the gray Pac-Man shapes. As the name suggests, cholinesterase inhibitors prevent cholinesterase from hydrolyzing acetylcholine into choline and acetate. This prolongs the life of acetylcholine in the synapse, which increases the activation of postsynaptic cholinergic receptors. This slows the memory loss caused by the deterioration of acetylcholine neurons in the hippocampus.
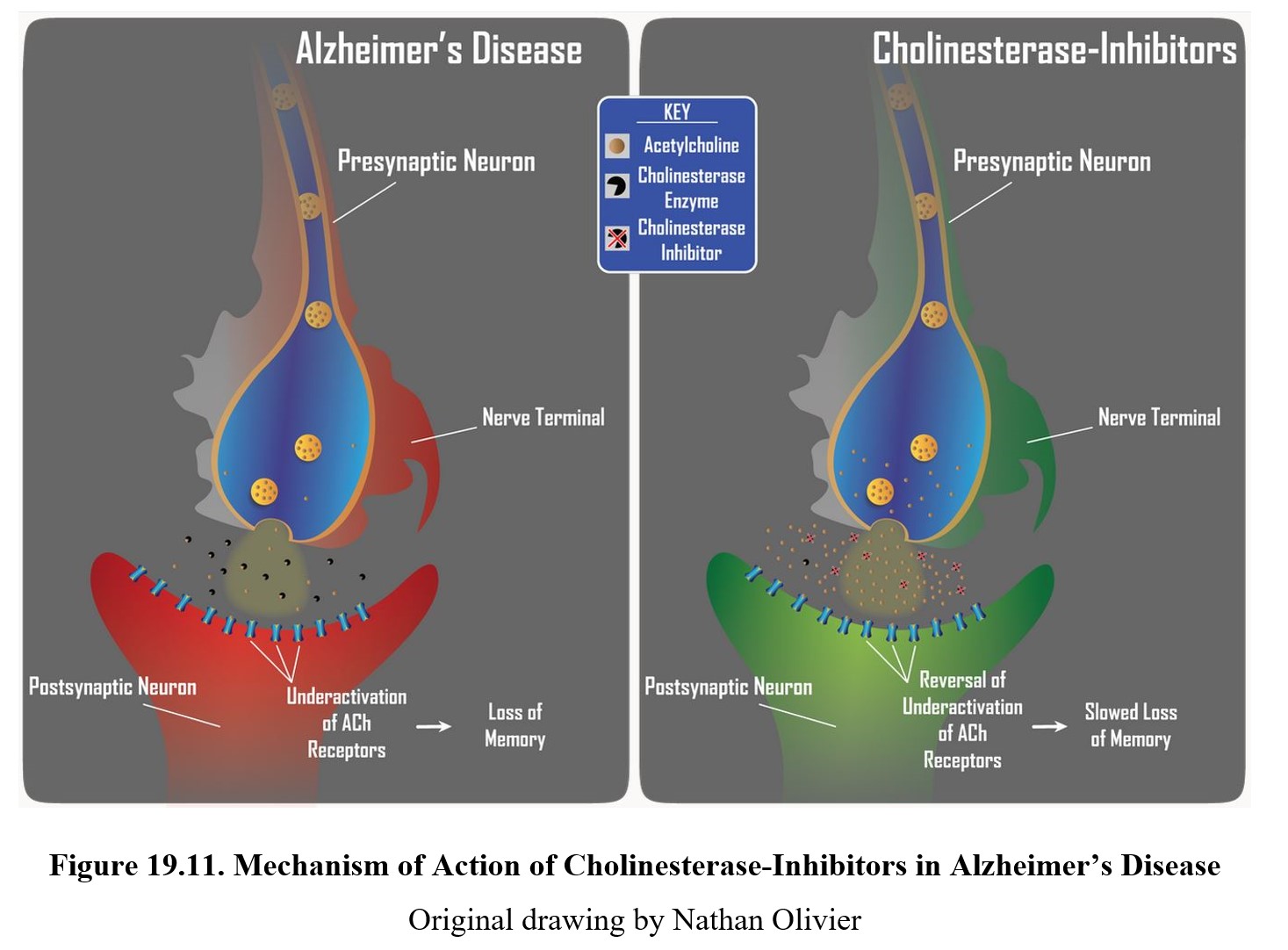
These drugs only slow the loss of memory since they do not prevent the continuing degradation of neurons. As more cells in the hippocampus die, cholinesterase inhibitors lose their effectiveness. Because of this, they are most effective in treating mild-to-moderate Alzheimer’s disease.
There are three cholinesterase inhibitors commonly prescribed: donepezil (Aricept®), rivastigmine (Exelon®), and galantamine (Razadyne®). Depending on the formulation, these drugs may come as pills, dissolvable tablets, or as transdermal patches. They all have similar side effects caused by increased acetylcholine activity, including low heart rate and blood pressure, nausea, vomiting, diarrhea, insomnia, dizziness, weight loss, and seizures. Because of the severity of the side effects, these drugs are usually not prescribed for the mild cognitive impairment that can proceed Alzheimer’s disease.
19.4.2. Memantine
For moderate to severe Alzheimer’s, a more effective drug is memantine. Memantine (Namenda®) is a noncompetitive NMDA antagonist that helps prevent glutamate-induced excitotoxicity. Recall that excitotoxicity is caused by high levels of calcium ions in the neuron. By blocking NMDA binding sites, memantine prevents the ion channels from opening and reduces the number of calcium ions that can enter the cell (see figure below).
Because it slows down the rate of neuron damage and death, memantine can prolong the transition from middle-stage Alzheimer’s to late-stage, increasing the amount of time patients can take care of some of their daily functions. Memantine has less of an effect on early-stage Alzheimer’s, as glutamate-induced excitotoxicity plays a smaller role in the progression of the disease and symptoms at that stage.
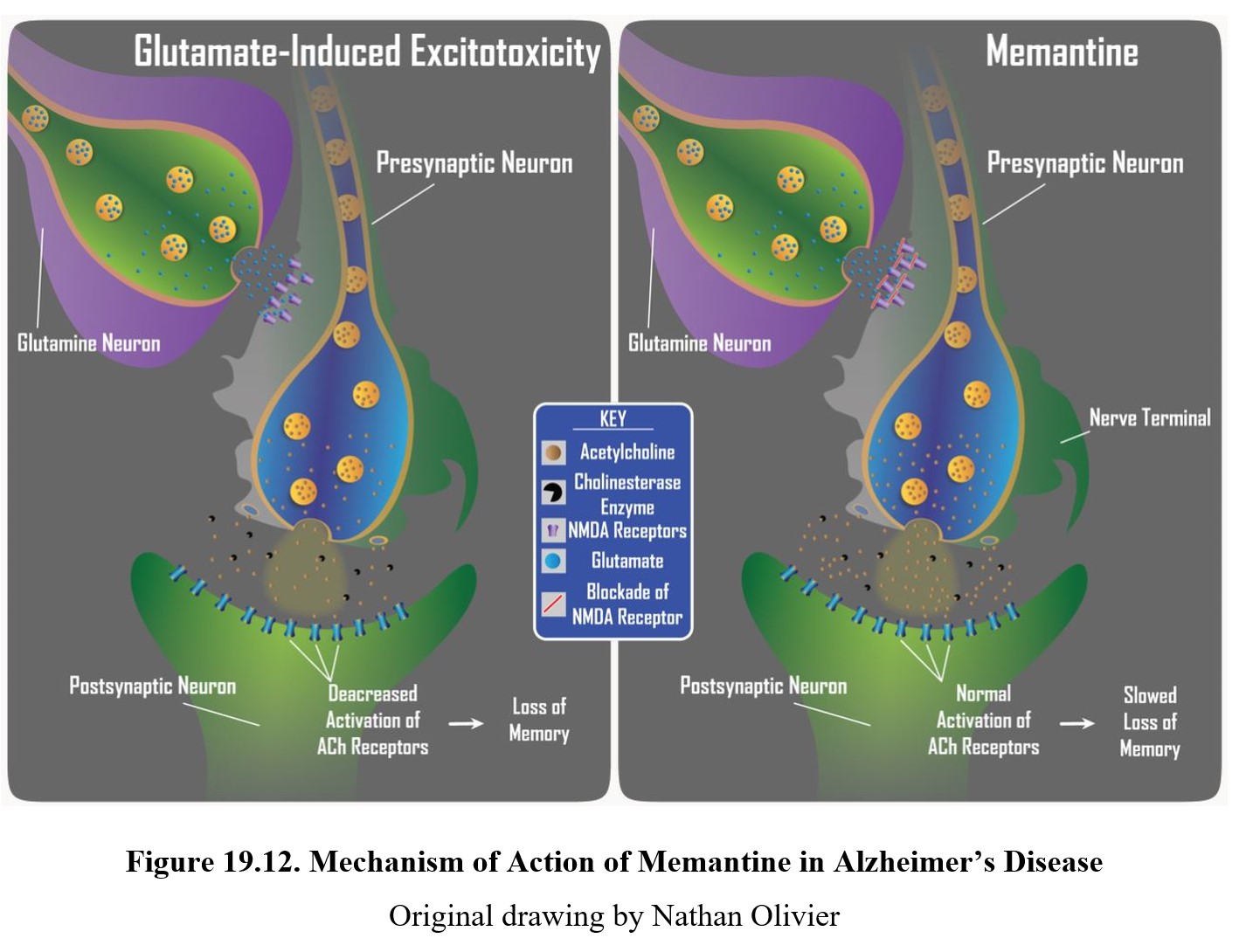
Similar to cholinesterase inhibitors, memantine can cause unpleasant side effects in some patients. These include nausea, vomiting, dizziness, drowsiness, insomnia, and anxiety. At very high doses memantine acts as a dissociative anesthetic, although the drug is not regularly misused as a psychoactive drug because it does not appear to cause euphoria or hallucinations.
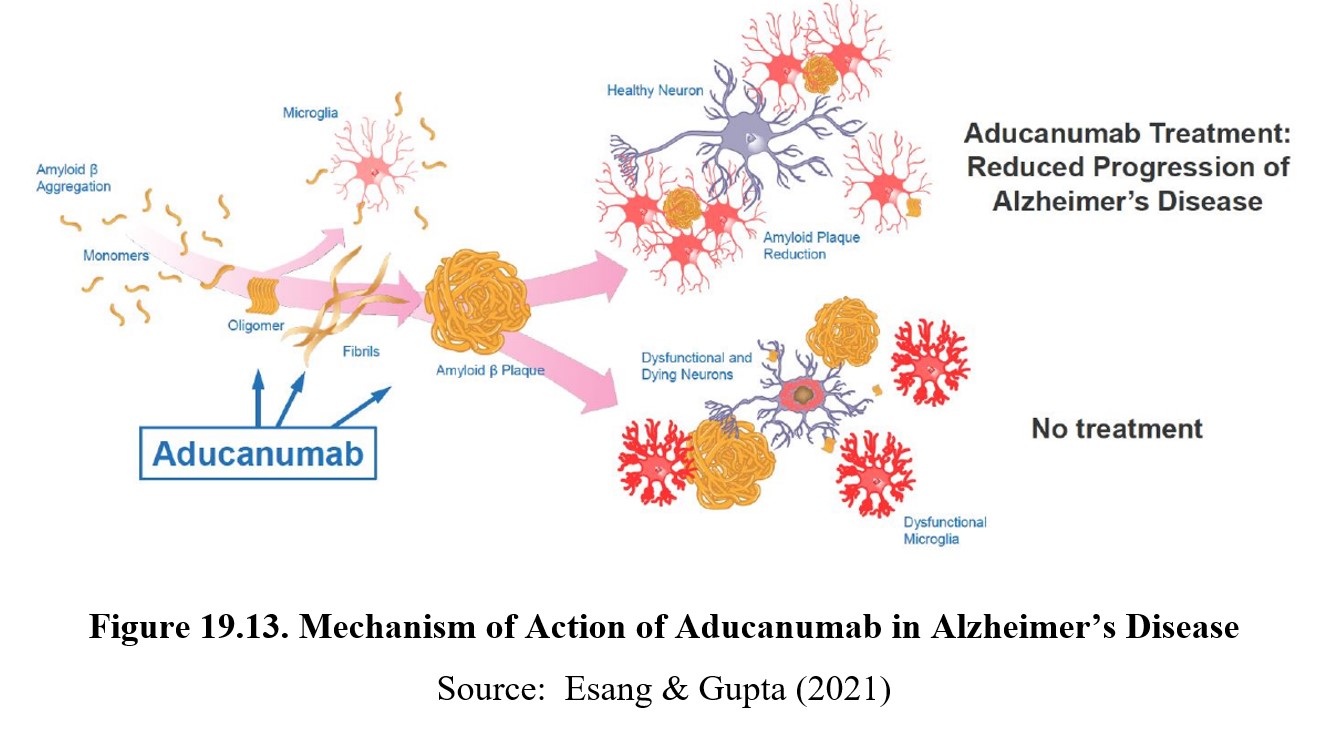
19.4.3. Aducanumab (Aduhlem®)
Newly approved in June 2021, aducanumab (Aduhlem®) is a monoclonal antibody directed against amyloid-beta which is thought to be a pathological cause of Alzheimer’s disease. This is a novel treatment for Alzheimer’s and is the first therapy that targets the basic pathophysiology of the disease. The drug manufacturer has announced a list price of $56,000 per year. The approval was controversial because an independent FDA advisory panel did not recommend approval because of conflicting results from clinical trials. The findings on whether aducanumab removes amyloid-beta from the brain were equivocal. The approval of the drug was followed by resignations from the FDA advisory panel. The accelerated FDA approval was conditional pending Phase 4 clinical trials to verify efficacy of aducanumab to cause cognitive improvement in Alzheimer patients.
Chapter Summary and Review
In this chapter, we covered ADHD and Alzheimer’s disease. We began our discussion of ADHD by defining the different types of ADHD and their diagnostic criteria, then explored some of the possible causes of ADHD. We followed this by explaining how norepinephrine and dopamine are thought to be involved in ADHD symptoms, as well as two types of drugs used to treat ADHD and how they are sometimes misused. For the second half of the chapter, we discussed Alzheimer’s disease, distinguishing it from other types of dementias and describing its three stages of progression. We learned about how amyloid plaques and neurofibrillary tangles may contribute to neurodegeneration, then explained how acetylcholine and glutamate may interact with this process. Finally, we discussed two types of Alzheimer’s medications that can slow the progression of the disease and provide some relief from its symptoms. A new monoclonal antibody against beta-amyloid is the first targeted therapy for Alzheimer’s.
Chapter 19 Practice Questions
Answer the following questions:
- Is ADHD more likely to be diagnosed in boys or girls?
- What are the three types of ADHD?
- What non-genetic factors might contribute to ADHD? Provide three examples of environmental factors that are linked to an increased risk, as well as three factors that do not show a link.
- What are executive functions? Describe how ADHD might impair them, including the neurotransmitters and brain regions involved.
- Explain how stimulants can treat ADHD.
- Can stimulants be prescribed for long-term treatment of ADHD? Why or why not?
- Describe the difference between atomoxetine and stimulants. Which is preferred for treating ADHD?
- Do medications like Adderall® or Ritalin® increase cognitive function in people without ADHD? Explain.
- Define dementia and provide four examples.
- Describe the three stages of Alzheimer’s disease. At which stage will people start to have difficulty recalling memories about their past?
- What are two pathological indicators of Alzheimer’s disease?
- What is a microtubule? What causes them to form neurofibrillary tangles?
- Can cholinesterase inhibitors reverse Alzheimer’s disease? Explain.
- Describe how apoptosis is triggered and what each step of the process entails.
- Explain the mechanism of action of memantine.
- What is aducanumab and why is it controversial?
2nd edition